Bartholin Gland Cancer
Bartholin Gland Cancer: Understanding a Rare Vulvar Malignancy
- What Is the Bartholin Gland?
- How Rare Is Bartholin Gland Cancer?
- What Causes Bartholin Gland Cancer?
- Symptoms and Clinical Presentation
- How Bartholin Gland Cancer Is Diagnosed
- Histologic Types and Staging of Bartholin Cancer
- Differences Between Benign and Malignant Bartholin Growths
- How ICD-10 Classifies Rare Vulvar Cancers
- Treatment Options and Surgical Approaches
- Survival Rates and Long-Term Outcomes
- Bartholin Cancer Recurrence and Follow-Up Protocol
- Bartholin Gland Cancer vs. Basal Cell Carcinoma
- Emotional and Psychological Impact
- Sexual Health and Recovery After Surgery
- Support Organizations and Educational Resources
- FAQ – Bartholin Gland Cancer
What Is the Bartholin Gland?
The Bartholin glands are two small, oval-shaped glands located on either side of the vaginal opening. Their primary role is to produce mucus that helps lubricate the vulva during sexual activity. These glands are typically no larger than a pea and are not noticeable unless inflamed or blocked.
Despite their essential function, these glands can sometimes develop issues, including cysts, infections, or in very rare cases, malignant tumors. Bartholin gland cancer represents less than 1% of all female genital cancers, making it both rare and challenging to diagnose early.
To differentiate this condition from more common benign growths, it’s important to understand the anatomy and behavior of these glands over time.
How Rare Is Bartholin Gland Cancer?
Bartholin gland carcinoma is extremely rare, accounting for a minute fraction of all gynecological malignancies. Due to its low incidence, it is often misdiagnosed as a benign Bartholin cyst or abscess, delaying correct treatment.
| Cancer Type | Estimated Incidence per 100,000 Women | Common Age Range | Prognosis (5-Year Survival) |
| Bartholin Gland Cancer | <0.1 | 50–70 years old | ~70% (if localized) |
| Vulvar Squamous Cell Carcinoma | 2.0 | 60+ | ~60–80% |
| Vaginal Adenocarcinoma | <0.2 | 40–60 | ~50–70% |
Most patients are diagnosed postmenopause, and tumors are usually detected during evaluation for persistent swelling or mass in the Bartholin gland region.
What Causes Bartholin Gland Cancer?
The precise cause of Bartholin gland cancer is unknown, but researchers believe a combination of genetic mutations, hormonal changes, and chronic inflammation could be contributing factors. Some cases have also shown associations with HPV (human papillomavirus), especially in squamous cell variants.
| Suspected Risk Factors | Possible Role in Development |
| Chronic Bartholin gland infections | May lead to cellular dysplasia |
| HPV infection (types 16, 18) | Possible trigger in squamous cell types |
| Age over 50 | Aging tissue may have lower immune defense |
| Smoking | Carcinogenic exposure to mucosal cells |
| Genetic mutations in tumor suppressor genes | Alters normal cell cycle control |
However, unlike cervical cancer, HPV is not a definitive cause in most cases. Much more research is required to confirm causative links.
Symptoms and Clinical Presentation
In its early stages, Bartholin gland cancer may mimic a simple cyst, which is why persistent or recurrent gland swelling should always be evaluated thoroughly. Symptoms often depend on the tumor’s size and location.
Infographic: Common Symptoms of Bartholin Gland Cancer
- A firm lump near the vaginal opening (usually one-sided)
- Pain or discomfort during sitting or intercourse
- Vaginal bleeding not related to menstruation
- Foul-smelling discharge (less common)
- Difficulty walking or urinating (in advanced cases)
- Enlarged lymph nodes in the groin
Unlike a typical abscess or cyst, cancerous masses are usually fixed to surrounding tissue, may ulcerate, and do not drain spontaneously.
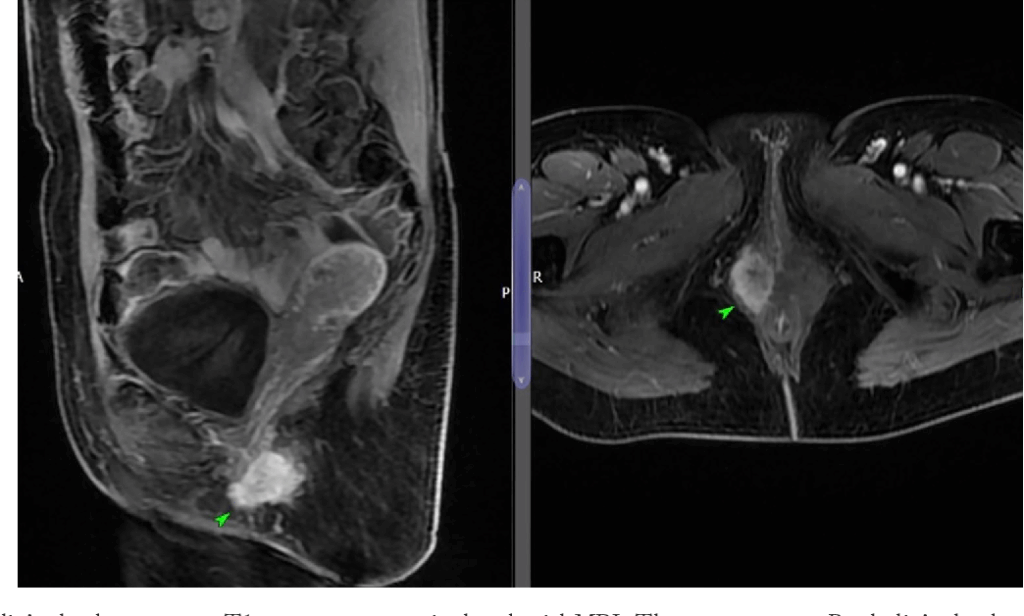
How Bartholin Gland Cancer Is Diagnosed
Because Bartholin gland cancer often mimics benign cysts or abscesses, accurate diagnosis can be delayed. A proper diagnosis typically involves a combination of physical examination, imaging, and biopsy.
| Diagnostic Method | Purpose | Notes |
| Pelvic examination | Assesses size, consistency, and mobility | Fixed, firm mass raises suspicion |
| Ultrasound | Differentiates cystic from solid lesions | Solid or mixed echogenicity may suggest malignancy |
| MRI or CT scan | Evaluates tumor extent and lymph node involvement | Useful for staging and surgical planning |
| Biopsy (needle or surgical) | Confirms histologic type | Gold standard for diagnosis |
| Lymph node assessment | Checks for metastasis | May require fine-needle aspiration |
Early detection significantly improves outcomes, but it often requires a high index of suspicion, especially in women over 40 presenting with persistent swelling in the Bartholin area.
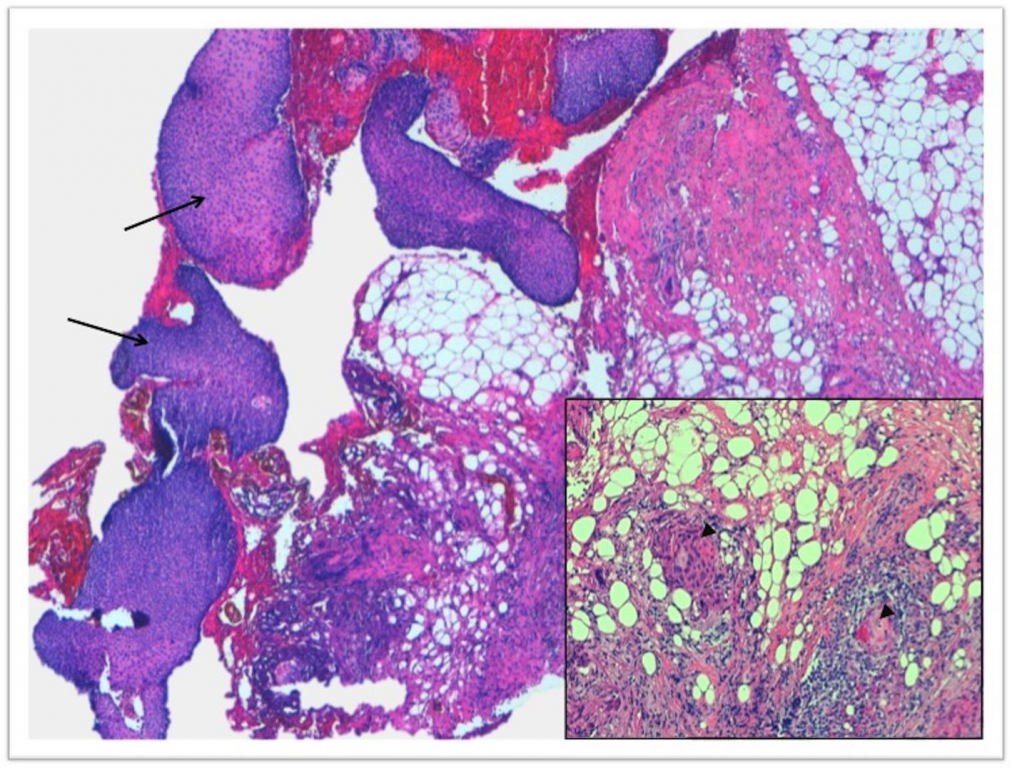
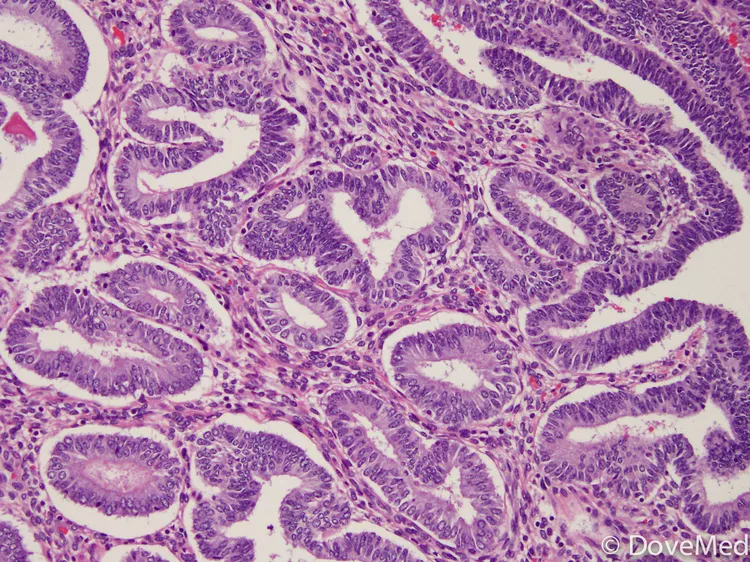
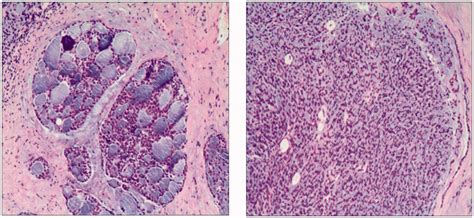
Histologic Types and Staging of Bartholin Cancer
Bartholin gland cancers come in several histologic subtypes. The most common is adenocarcinoma, followed by squamous cell carcinoma and adenoid cystic carcinoma. Each type behaves differently and influences treatment decisions.
| Histologic Type | Frequency | Characteristics |
| Adenocarcinoma | ~40–50% | Arises from glandular tissue; slow-growing |
| Squamous cell carcinoma | ~20–30% | HPV-associated; more aggressive |
| Adenoid cystic carcinoma | ~10–15% | High risk of perineural invasion; recurrence prone |
| Transitional cell carcinoma | Rare | Unusual presentation, resembles bladder cancer |
Staging follows the FIGO system for vulvar cancers, focusing on tumor size, depth of invasion, lymph node involvement, and distant metastasis. Early-stage cancers (I–II) have a much better prognosis than advanced stages.
Differences Between Benign and Malignant Bartholin Growths
Distinguishing between benign Bartholin gland cysts and malignant tumors is essential for early cancer detection. The table below compares key clinical and imaging characteristics:
| Feature | Benign Cyst | Malignant Tumor |
| Onset | Often acute | Gradual, persistent |
| Pain | Tender if infected | May be painless or cause dull discomfort |
| Consistency | Soft, fluid-filled | Firm, irregular |
| Mobility | Freely movable | Fixed to surrounding structures |
| Age of onset | Often <40 years | Most cases >50 years |
| Imaging appearance | Anechoic on ultrasound | Solid or mixed echogenicity |
Persistent, non-resolving masses in older women should always be biopsied. Misdiagnosis can delay crucial treatment.
How ICD-10 Classifies Rare Vulvar Cancers
Bartholin gland cancer is officially classified within the ICD-10 coding system under the broader category of malignant neoplasms of the vulva, specifically:
| ICD-10 Code | Description |
| C51.0 | Malignant neoplasm of labium majus |
| C51.1 | Malignant neoplasm of labium minus |
| C51.2 | Malignant neoplasm of clitoris |
| C51.8 | Overlapping lesions of vulva |
| C51.9 | Malignant neoplasm of vulva, unspecified |
There is no specific code for Bartholin gland cancer itself. Instead, tumors are usually coded as C51.9 or C51.8, depending on location.
Treatment Options and Surgical Approaches
Treatment of Bartholin gland cancer is typically surgical, often combined with radiation or chemotherapy depending on the cancer’s stage and type. Because of its rare and variable nature, therapy is personalized.
| Treatment Modality | Use Case | Notes |
| Wide local excision | Early-stage, localized tumors | Preserves vulvar anatomy if margins are clear |
| Radical vulvectomy | Advanced tumors or poor margin control | May be partial or total depending on spread |
| Inguinofemoral lymphadenectomy | If nodes are enlarged or suspicious | Commonly bilateral if high-grade tumor |
| Radiotherapy | Postoperative in case of margin positivity or nodal spread | External beam radiation used most often |
| Chemotherapy | Rarely first-line; may be used for metastasis | Cisplatin or 5-FU-based regimens are common |
Minimally invasive techniques are not typically used due to anatomical complexity and proximity to the vaginal and anal sphincters.
Survival Rates and Long-Term Outcomes
Prognosis depends heavily on tumor size, lymph node status, and histologic subtype. When detected early and treated surgically, outcomes are relatively favorable. Late-stage tumors or those with lymph node involvement carry a worse outlook.
| Stage of Cancer | Approx. 5-Year Survival Rate | Notes |
| Stage I | ~80–90% | Localized to Bartholin gland |
| Stage II | ~65–75% | Spread to nearby tissue, not nodes |
| Stage III | ~40–60% | Inguinal lymph node involvement |
| Stage IV | <30% | Distant metastasis (e.g., lungs, liver) |
Adenoid cystic carcinoma, though slow-growing, tends to recur even after initial treatment, which necessitates long-term follow-up over 10 years or more.
Bartholin Cancer Recurrence and Follow-Up Protocol
Patients treated for Bartholin gland cancer require structured long-term follow-up. Recurrence may happen locally (in the vulva) or distantly (lungs, liver, lymph nodes). Most recurrences occur within the first 2–3 years.
Infographic: Follow-Up Timeline
- Every 3–4 months for the first 2 years
- Every 6 months from years 3 to 5
- Annually thereafter
- Imaging (CT/MRI) as indicated by symptoms
- Pelvic exam at each follow-up
| Monitoring Approach | Purpose |
| Clinical examination | Detect local recurrence |
| Imaging (as needed) | Rule out deep pelvic or distant metastases |
| Biopsy (if suspicious lesion) | Confirm recurrent malignancy |
Patient education on self-awareness of symptoms (e.g., new masses, pain, or discharge) is critical for early detection of recurrence.
Bartholin Gland Cancer vs. Basal Cell Carcinoma
Though both may appear as vulvar skin lesions, Bartholin gland cancer and basal cell carcinoma (BCC) have distinct origins, behaviors, and treatments. Misidentifying one for the other can delay effective therapy.
| Feature | Bartholin Gland Cancer | Basal Cell Carcinoma |
| Cell origin | Glandular or squamous epithelium | Basal cells of the skin |
| Common location | Inside vulvar vestibule | Outer labia or perineum |
| Appearance | Firm, submucosal mass | Pearly, ulcerated skin lesion |
| Metastasis risk | Moderate (esp. to lymph nodes) | Very low |
| Treatment | Surgery ± radiation or chemo | Local excision, rarely requires more |
Emotional and Psychological Impact
A diagnosis of Bartholin gland cancer can be emotionally destabilizing, particularly because of the cancer’s location in a highly personal and intimate area. Patients may feel fear, shame, or isolation, especially if the diagnosis is delayed due to misinterpretation as a benign cyst.
Key Emotional Challenges:
| Psychological Impact | Description |
| Anxiety and fear | Uncertainty about treatment outcomes and recurrence |
| Body image concerns | Surgery may cause physical changes affecting confidence |
| Sexual identity disruption | Altered sense of femininity and self-esteem |
| Isolation | Due to rarity, few peer connections or public awareness |
Mental health support is essential. Counseling, peer support groups, and open communication with healthcare providers can significantly improve emotional resilience.
Sexual Health and Recovery After Surgery
Surgical treatment, especially vulvectomy or lymphadenectomy, may have long-term consequences for sexual function. These may include physical discomfort, scarring, or changes in vaginal lubrication and sensation.
| Aspect of Sexual Health | Possible Changes After Treatment |
| Vaginal dryness | Due to gland removal or nerve damage |
| Pain during intercourse | Related to scarring, tightness, or fear |
| Libido fluctuations | From stress, fatigue, or hormonal effects |
| Partner communication | Often requires reassurance and mutual understanding |
Recovery plans should incorporate pelvic floor physical therapy, gentle sexual reintroduction strategies, and when needed, vaginal dilators or lubricants. Honest communication with partners is crucial for maintaining intimacy.
Support Organizations and Educational Resources
Because Bartholin gland cancer is rare, many patients feel underserved or under-informed. Fortunately, several organizations provide educational content, patient advocacy, and peer connection opportunities.
| Organization | Role and Services Offered |
| National Vulvar Cancer Support Network | Community support, survivor stories, resources |
| CancerCare | Free counseling, financial assistance |
| Foundation for Women’s Cancer | Medical updates, patient webinars, clinical trials |
| American Cancer Society | General support, educational material |
These resources help patients make informed decisions, connect with others, and navigate the complexities of treatment and recovery.
FAQ – Bartholin Gland Cancer
1. Can Bartholin gland cancer occur in younger women?
Yes, though it is rare. While most cases are diagnosed in postmenopausal women, younger patients can develop this cancer, especially with certain histologic types like adenoid cystic carcinoma.
2. Is Bartholin gland cancer linked to STDs?
There is limited evidence. HPV (a sexually transmitted virus) may play a role in some subtypes, particularly squamous cell carcinoma, but it is not a definitive cause.
3. How fast does Bartholin gland cancer grow?
Growth rate varies. Adenoid cystic tumors are slow-growing but locally aggressive. Squamous cell variants may progress more quickly and involve lymph nodes earlier.
4. Can this cancer be treated without removing the gland?
In most cases, removal of the gland is required for clear margins. Conservative surgery may be attempted for very small, localized tumors, but this is uncommon.
5. Is recurrence common?
Yes, especially in adenoid cystic types. Even with negative margins, recurrence can occur years later. Long-term monitoring is critical.
6. Can Bartholin gland cancer be found on a Pap smear?
No. Pap smears screen for cervical cancer, not vulvar or Bartholin gland malignancies. Bartholin tumors are often missed unless biopsied directly.
7. Is radiation always required?
Not always. It depends on tumor size, grade, and lymph node involvement. Early-stage tumors with clean margins may not require radiation.
8. What does Bartholin gland cancer feel like?
It usually presents as a firm, painless lump that doesn’t go away. Unlike a cyst, it’s often fixed and does not respond to antibiotics.
9. Can imaging alone diagnose this cancer?
No. Imaging can help assess the mass but cannot confirm malignancy. A biopsy is essential for diagnosis.
10. Can Bartholin gland cancer spread to other organs?
Yes, though not common in early stages. Advanced disease can metastasize to the lungs, liver, or pelvic lymph nodes.
11. Is it hereditary?
There’s no strong evidence of hereditary patterns, but a personal or family history of gynecological cancers may warrant more careful monitoring.
12. Can hormone therapy affect Bartholin gland cancer?
There’s no direct link, but hormone-responsive tumors may be influenced by estrogen levels. Always consult an oncologist before initiating HRT.
13. Are there clinical trials for this cancer?
Few exist due to its rarity, but some trials for vulvar or rare gynecologic cancers may include eligible patients. Ask your oncologist to search trial registries.
14. Can a Bartholin cyst turn into cancer?
Rarely. Long-standing cysts or those that frequently recur should be evaluated, especially in women over 40, but direct transformation is uncommon.
15. What are warning signs for recurrence?
Any new lump, pain, or unusual discharge in the vulvar area—especially on the previously treated side—should prompt immediate medical evaluation.









