What Does Ovarian Cancer Leg Pain Feel Like?
What Does Ovarian Cancer Leg Pain Feel Like? Full Guide for Beginners
- Why Leg Pain May Be a Hidden Sign of Ovarian Cancer
- The Nature of Ovarian Cancer Leg Pain: Key Characteristics
- How Leg Pain Develops in Ovarian Cancer: Understanding the Physiology
- Comparing Ovarian Cancer Leg Pain with Other Types of Leg Pain
- Duration and Timing: How Long Leg Pain May Appear Before Diagnosis
- Location-Specific Symptoms: Where the Pain Is Usually Felt
- Leg Swelling, Numbness, and Other Sensory Clues
- Does the Pain Worsen Over Time?
- Misdiagnosis: Conditions Commonly Confused with Ovarian Cancer Leg Pain
- Leg Pain Without Abdominal or Pelvic Symptoms: Is It Still Cancer?
- When to See a Doctor About Leg Pain
- Imaging and Diagnostic Tools for Ovarian Cancer-Linked Leg Pain
- Treatment Options Once Ovarian Cancer Is Diagnosed
- Managing Leg Pain During Ovarian Cancer Treatment
- When Leg Pain Signals Recurrence of Ovarian Cancer
- Emotional Impact and Public Awareness of Ovarian Cancer Leg Pain
- FAQ – 15 Questions About Ovarian Cancer and Leg Pain Not Answered Above
Why Leg Pain May Be a Hidden Sign of Ovarian Cancer
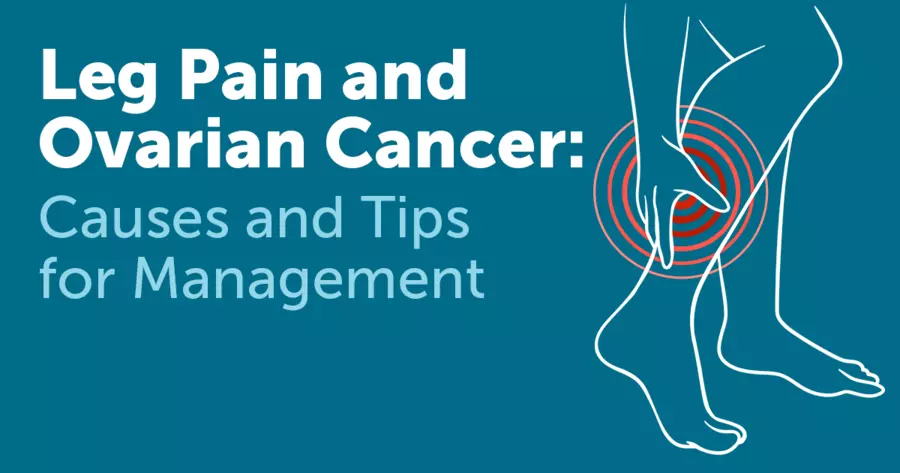
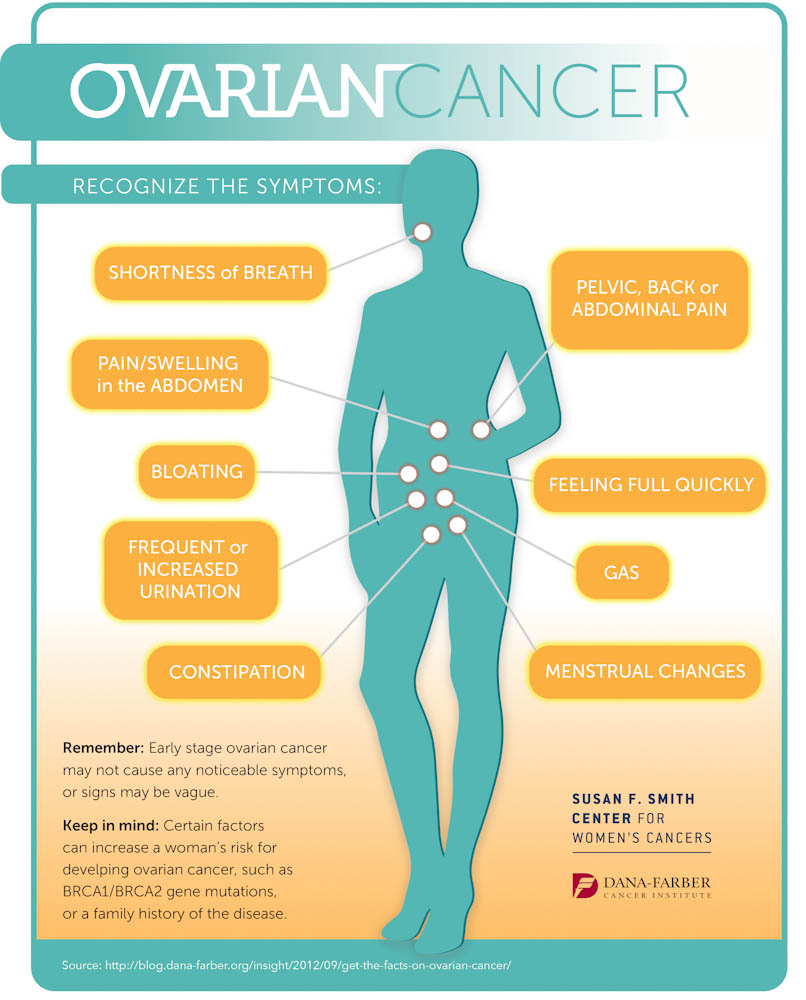
Ovarian cancer is often called the “silent killer” due to its vague and nonspecific symptoms. While abdominal discomfort and bloating are commonly discussed, leg pain is a lesser-known yet important early indicator. Many women report persistent aching, pressure, or unusual sensations in the legs, which can precede a diagnosis by months.
This leg pain is not typically muscular or orthopedic in origin. Instead, it may result from pressure placed by ovarian tumors on surrounding lymphatic structures, nerves, or blood vessels. Recognizing how this type of pain differs from more common causes can play a key role in early detection. In some cases, it may be the only noticeable symptom before more obvious signs of cancer develop — highlighting the need to cross-reference with the Updated List of Cancer Symptoms.
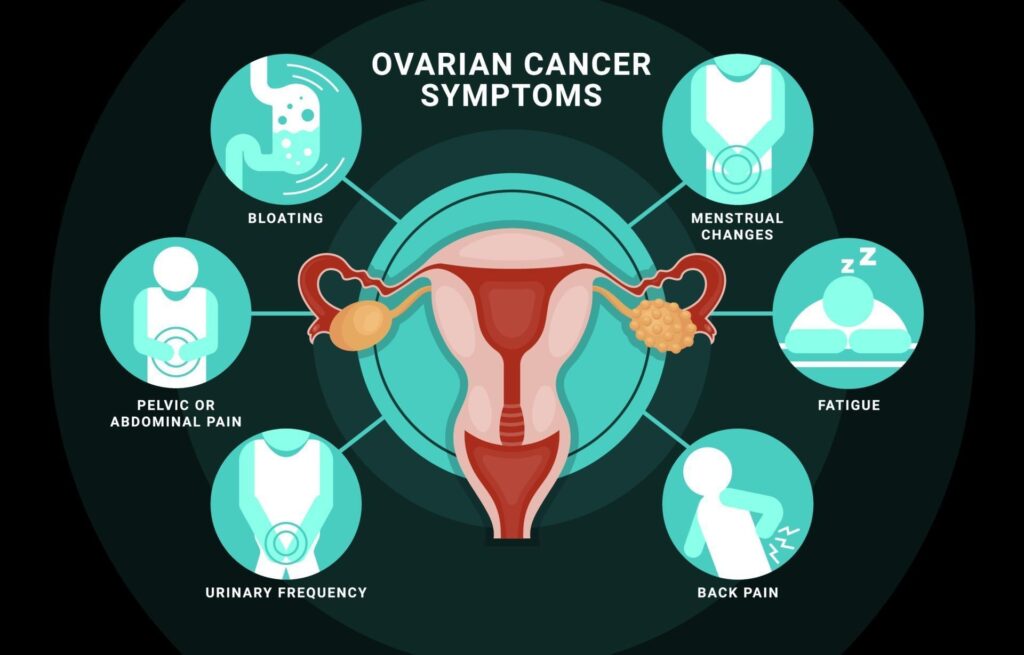
The Nature of Ovarian Cancer Leg Pain: Key Characteristics
Unlike pain from injury or arthritis, leg pain associated with ovarian cancer is often described as deep, aching, or heavy. It may feel persistent rather than sharp or shooting, although nerve involvement can lead to radiating discomfort.
| Sensation Reported | Description |
| Deep aching | A heavy, dull discomfort felt in the thigh or calf, often worse at night |
| Pressure or fullness | A sensation that the leg is swollen or under compression |
| Burning or tingling | May occur if nearby nerves are affected or compressed |
| Unilateral pain | Typically affects only one leg, especially when linked to tumor pressure |
| No clear injury or cause | Appears without exercise, strain, or trauma |
This type of pain is often mistaken for sciatica, restless leg syndrome, or circulatory problems. However, when these sensations persist despite rest or physical therapy, further gynecological evaluation is warranted.
How Leg Pain Develops in Ovarian Cancer: Understanding the Physiology
Ovarian tumors, especially in later stages, can grow large enough to exert pressure on the pelvic nerves, lymphatic vessels, and major veins that drain the lower body. When these structures are compressed, they cause altered blood flow and nerve signaling — both of which contribute to leg discomfort.
Infographic: How Tumors Cause Leg Pain
- Tumor grows in the pelvic cavity
- Compresses nearby iliac veins or lymph nodes
- Leads to restricted venous return from the legs
- Causes pooling of blood and interstitial fluid
- Results in heaviness, swelling, and aching pain in the affected limb
In advanced cases, deep vein thrombosis (DVT) may develop, increasing the urgency for diagnosis and intervention.
Comparing Ovarian Cancer Leg Pain with Other Types of Leg Pain
It’s important to distinguish ovarian cancer-related pain from other sources like muscular strain, vascular issues, or nerve compression. This distinction often determines whether patients receive early or delayed care.
| Condition | Key Features of Leg Pain |
| Ovarian Cancer | Dull, aching, often unilateral; linked to pelvic fullness or bloating |
| Sciatica | Sharp, radiating pain from lower back to foot; worsens with movement |
| DVT (blood clot) | Sudden swelling, warmth, and tenderness; often with redness |
| Varicose veins | Cramping and heaviness, especially after standing; visual vein changes |
| Muscle strain | Localized pain post-activity; resolves with rest |
Knowing how to compare these types helps both patients and doctors prioritize the right imaging and referrals — especially when cancer is still a possibility. Further awareness of general Warning Signs of Cancer may support early action.
Duration and Timing: How Long Leg Pain May Appear Before Diagnosis

One of the challenges in detecting ovarian cancer early is the subtle and prolonged nature of its symptoms. Leg pain may develop weeks or even several months before diagnosis, especially in women with slow-growing or asymptomatic tumors.
| Stage of Pain Onset | Observations from Patients and Studies |
| 1–2 weeks | May be dismissed as fatigue or overuse |
| 3–6 weeks | Persistent aching noticed during rest or sleep |
| 2–6 months | Unresolved pain becomes chronic; initial misdiagnoses common |
| Post-diagnosis | Often improves after surgery or targeted treatment |
Patients frequently report that the pain becomes part of their daily life before other symptoms like bloating or urinary changes appear. This delay can result in late-stage detection, underscoring the need for improved public education on early indicators.
Location-Specific Symptoms: Where the Pain Is Usually Felt
The sensation of ovarian cancer-related leg pain is often localized rather than diffuse. It tends to focus on certain regions depending on tumor size, location, and lymphatic involvement.
Infographic: Common Leg Pain Locations in Ovarian Cancer
- Inner thigh (unilateral): Most frequently affected due to lymph node compression
- Back of calf: Heaviness or pressure sensation from venous congestion
- Buttock and hip region: If sacral nerves or pelvic muscles are affected
- Knee area: Referred pain or nerve involvement mimicking orthopedic conditions
- Foot (numbness/tingling): Late sign due to nerve compression in advanced stages
Because the discomfort is commonly felt on one side only, it may lead to misdiagnosis as a localized muscle strain or sciatica. Bilateral pain is less common unless both iliac vessels or nerves are compromised.
Leg Swelling, Numbness, and Other Sensory Clues
Beyond aching, patients may notice visible swelling, changes in skin temperature, or unusual tingling sensations. These signs typically reflect impaired lymphatic or venous flow, caused by tumor obstruction in the pelvis or abdomen.
| Symptom Type | Description and Clinical Meaning |
| Visible swelling | Soft tissue enlargement in thigh or lower leg; often unilateral |
| Tingling or numbness | Sensory changes from nerve pressure; may worsen with prolonged sitting |
| Skin warmth | Could indicate clot formation or inflammation |
| Fatigue or heaviness | Difficulty standing or walking long distances |
| Tense skin | Edema buildup; often worsens toward evening or after prolonged standing |
These symptoms may resemble vascular or neurological conditions but don’t respond to typical treatment unless the underlying tumor is addressed.
Does the Pain Worsen Over Time?
For many patients, the pain increases gradually, tracking tumor growth and lymphatic obstruction. Initially mild, it can become moderate to severe — particularly as tumor size begins to affect more internal structures or as fluid builds up in the abdominal cavity.
Infographic: Progression of Ovarian Cancer Leg Pain
- Stage I–II: Pain is intermittent, usually mild
- Stage III: Becomes daily, heavier, may require analgesics
- Stage IV: Can become disabling, especially with DVT or lymphedema
- Post-treatment: May improve significantly with tumor removal
Unlike acute trauma, which improves with rest, this pain tends to intensify even in stillness or at night — a key distinction that helps alert clinicians to deeper causes.
Misdiagnosis: Conditions Commonly Confused with Ovarian Cancer Leg Pain
Because the pain pattern is often subtle and non-specific, it’s frequently misattributed to orthopedic or neurological issues. This can delay accurate diagnosis by months. Understanding how ovarian cancer-related leg pain is misread helps reduce misdiagnosis.
| Condition | Overlapping Symptoms | Key Differences From Ovarian Cancer Leg Pain |
| Sciatica | Radiating pain, numbness | Originates in lower back, worsens with posture |
| Arthritis | Stiffness, joint pain | Localized to joints, responds to anti-inflammatories |
| Varicose veins | Heaviness, mild swelling | Visible vein changes, improved by elevation |
| Muscle strain | Dull ache, tightness | Follows activity, resolves with rest |
| Peripheral neuropathy | Tingling, numbness | Often symmetrical and associated with diabetes |
These conditions can overlap with cancer-related symptoms, especially in older patients, which is why a comprehensive gynecologic and vascular evaluation is critical when the pain is persistent and unresponsive to treatment.
Leg Pain Without Abdominal or Pelvic Symptoms: Is It Still Cancer?
Yes — leg pain can occur in the absence of classic ovarian cancer symptoms. While abdominal bloating, changes in bowel habits, or frequent urination are more widely known, isolated leg pain has been reported in early and even advanced cases.
| Patient Scenario | Clinical Implication |
| Isolated leg pain for weeks | May be early sign of pelvic tumor impinging on nerves |
| No abdominal pain or bloating | Common in patients with posterior pelvic tumor growth |
| Referred pain from pelvic region | Nerve pathways may cause pain to appear far from tumor site |
| Normal pelvic exam results | Some tumors are deep and not palpable |
These findings reinforce that not all ovarian cancers present traditionally. Pain in the leg — especially when unexplained, one-sided, and chronic — should not be ignored even in the absence of pelvic complaints. To support broader vigilance, refer to the Updated List of Cancer Symptoms.
When to See a Doctor About Leg Pain
Women experiencing persistent, one-sided leg pain that does not improve with rest, exercise modification, or over-the-counter medications should consider a gynecological evaluation. The longer the pain persists, the greater the concern for possible pelvic pathology.
Infographic: When to Seek Medical Attention
- Leg pain lasting longer than 3 weeks
- Accompanied by bloating or urinary changes
- Increasing in intensity without obvious cause
- Present only on one side
- Not relieved by standard physical therapy or medications
- New onset of tingling, numbness, or swelling
These indicators do not automatically confirm cancer but warrant imaging and referral to rule out serious causes, including gynecological tumors.
Imaging and Diagnostic Tools for Ovarian Cancer-Linked Leg Pain
Once ovarian cancer is suspected, imaging is essential for confirming tumor presence, size, and compression effects. Several diagnostic tools are available depending on the suspected location and progression of disease.
| Imaging Type | Use Case in Leg Pain + Ovarian Cancer Evaluation |
| Transvaginal ultrasound | First-line imaging for ovarian structures |
| Pelvic MRI | High-resolution images of masses and surrounding tissues |
| CT scan (abdomen/pelvis) | Detects tumor size, lymph node involvement, and spread |
| Doppler ultrasound of leg | Rules out DVT as source of pain or swelling |
| PET-CT | Used in cancer staging and detection of metastasis |
These imaging techniques help distinguish ovarian tumors from other causes of leg symptoms and guide the next steps in treatment and referral. Additional context on overlapping conditions like Melanoma may be considered in differential diagnoses involving skin changes.
Treatment Options Once Ovarian Cancer Is Diagnosed
Once ovarian cancer is confirmed and identified as the cause of leg pain, treatment typically begins with a combination of surgery and chemotherapy. The goal is to remove as much of the tumor as possible (cytoreductive surgery), followed by systemic therapy to eliminate residual cancer cells.
| Treatment Type | Role in Reducing Tumor and Associated Leg Pain |
| Debulking surgery | Removes tumor mass and relieves pressure on nerves/vessels |
| Platinum-based chemotherapy | Shrinks remaining cancer cells and reduces lymphatic congestion |
| Targeted therapies | Used for tumors with genetic mutations (e.g., BRCA) |
| Radiation therapy | Less common, but may be used in recurrence involving pelvis |
As tumor burden decreases, the leg pain often subsides or disappears entirely, further confirming its direct link to mass effect or nerve irritation from cancer.
Managing Leg Pain During Ovarian Cancer Treatment
Pain management is essential during treatment, particularly in patients with advanced-stage disease. A multimodal strategy involving medications, physical therapy, and lifestyle modifications is commonly employed.
Infographic: Pain Management Toolkit
- Non-opioid medications (acetaminophen, NSAIDs) for mild discomfort
- Opioids or nerve stabilizers (gabapentin) for severe or nerve-related pain
- Compression garments to reduce swelling and venous pooling
- Lymphatic drainage techniques to reduce edema in lower limbs
- Guided physical therapy for maintaining mobility and reducing pressure
Pain control not only improves quality of life, but also helps maintain physical independence during therapy, which is strongly correlated with survival outcomes.
When Leg Pain Signals Recurrence of Ovarian Cancer
In survivors, the return of leg pain can sometimes signal cancer recurrence, particularly in the pelvic or lymph node regions. Regular follow-up care should always include discussion of any new or persistent lower body symptoms.
| Recurrence Indicator | Interpretation |
| Reappearance of leg pain | May indicate tumor regrowth or new compression |
| New swelling in one leg | Requires urgent DVT screening and imaging for mass effect |
| Pelvic pressure with leg heaviness | Common in recurrent tumors along the pelvic wall |
| Elevated CA-125 blood marker | May align with symptomatic return of discomfort |
Patients are encouraged to report any unusual or returning symptoms, even if minor, to their oncologist, as early detection of recurrence greatly improves treatment response.
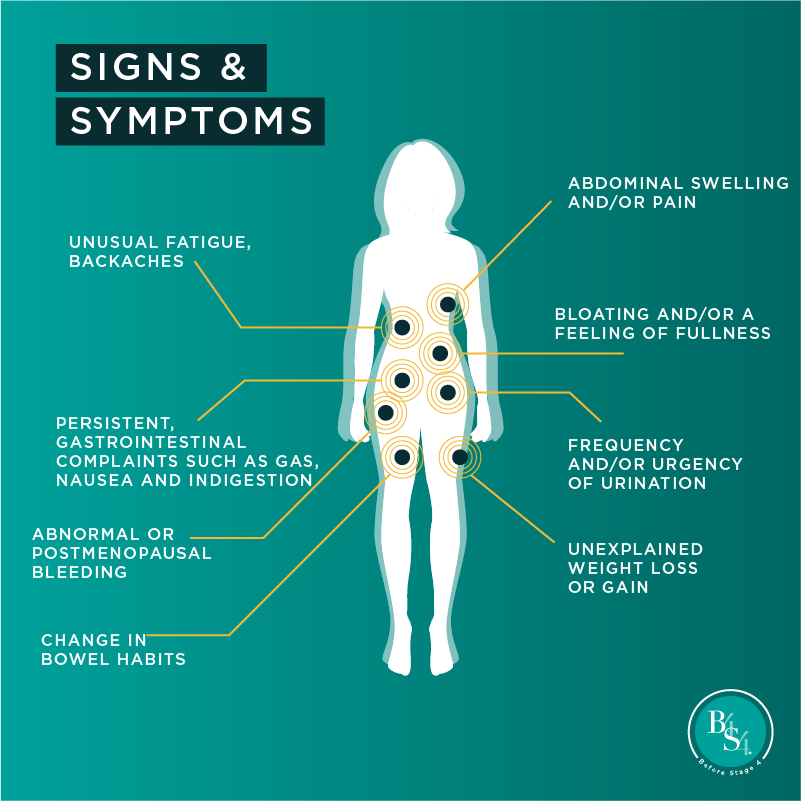
Emotional Impact and Public Awareness of Ovarian Cancer Leg Pain
Many women who experienced leg pain prior to diagnosis report frustration or guilt that they ignored it or had it misdiagnosed. The emotional toll of delayed diagnosis—paired with the physical burden of pain—highlights the need for public education.
| Aspect of Impact | Observed Effect on Patients and Survivors |
| Delayed diagnosis | Leads to self-blame or mistrust in the medical system |
| Persistent symptoms | Affect sleep, mood, and physical function |
| Social awareness gap | Many unaware that leg pain can be linked to gynecologic cancers |
| Advocacy role of survivors | Sharing personal stories to improve early recognition |
Awareness campaigns now emphasize non-gynecologic symptoms of ovarian cancer, such as leg pain, back pain, and fatigue, to ensure women seek help sooner. Cross-reference this with broader data in the Warning Signs of Cancer.
FAQ – 15 Questions About Ovarian Cancer and Leg Pain Not Answered Above
1. Can leg pain be the only symptom of ovarian cancer?
Yes, in some cases, persistent leg pain precedes other signs. This is especially true in early or deep pelvic tumors that haven’t yet caused abdominal symptoms.
2. What kind of doctor should I see for unexplained leg pain?
Start with your primary care provider or gynecologist. If cancer is suspected, you may be referred to a gynecologic oncologist and undergo imaging.
3. Does leg pain mean the cancer has already spread?
Not necessarily. It may simply result from localized tumor pressure. However, in advanced stages, leg symptoms may reflect lymphatic or vascular spread.
4. Can ovarian cysts cause similar leg pain?
Yes, large or ruptured cysts can cause nerve pressure or fluid accumulation mimicking cancer-related leg symptoms, but they are usually benign and resolve.
5. How quickly does leg pain go away after treatment?
Pain often improves within weeks after tumor reduction or surgical removal. In some cases, nerve-related symptoms may linger longer if damage occurred.
6. Is leg pain during ovarian cancer always one-sided?
Most often, yes. Unilateral symptoms are more typical, but bilateral pain can occur in advanced stages or if fluid builds up symmetrically.
7. Can exercise help alleviate ovarian cancer leg pain?
Light movement can improve circulation, but rigorous activity may worsen pain. Always follow a physical therapist’s guidance during treatment.
8. Is swelling more dangerous than the pain itself?
Swelling may indicate DVT or lymphatic obstruction, which are medical emergencies. Pain without swelling is usually less urgent but still important.
9. Are older women more likely to have leg pain from ovarian cancer?
Age is a risk factor for both ovarian cancer and poor circulation, but leg pain can occur at any age depending on tumor size and location.
10. Does pain occur during the night or rest periods?
Yes, many patients report worsening pain in the evening or when lying down due to fluid redistribution and nerve sensitivity.
11. What if imaging shows nothing but pain persists?
You may require more advanced scans (MRI or PET-CT). Deep pelvic tumors may not be visible on basic ultrasound or X-ray.
12. Could pain relievers mask symptoms and delay diagnosis?
They may relieve symptoms temporarily but don’t treat the root cause. Relying on medication alone without investigation is risky.
13. Can menopause cause similar leg pain?
Menopause can bring changes in circulation and muscle mass, but it doesn’t usually cause persistent unilateral pain linked to pressure effects.
14. Is numbness a worse sign than pain?
Numbness suggests nerve involvement and may reflect more advanced or strategically placed tumors. It requires immediate evaluation.
15. How do I talk to my doctor if I’m worried about cancer?
Be direct. Mention that your pain is unexplained, persistent, and you’re concerned about cancer. Request pelvic imaging or referral.









