Signs of Magnesium Deficiency in the Body: What to Watch For and How to Restore Balance
- What Is Magnesium and Why Your Body Depends on It
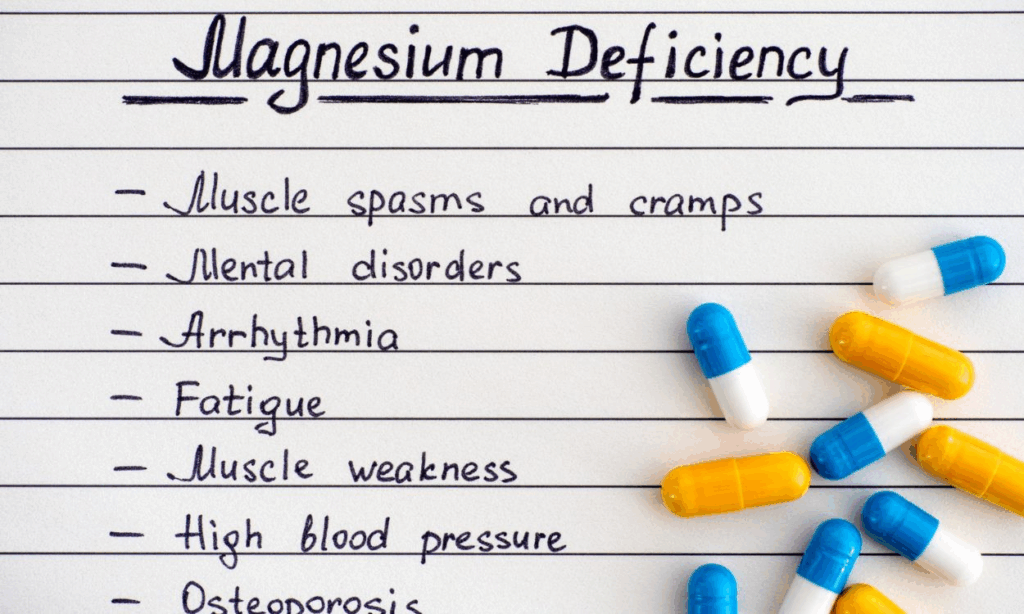
- Early Warning Signs of Magnesium Deficiency
- Advanced Symptoms of Prolonged Deficiency
- Physical, Emotional, and Neurological Symptoms Linked to Low Magnesium
- Hidden Causes of Magnesium Deficiency You Might Not Notice
- How Magnesium Deficiency Affects Sleep Quality
- Magnesium Deficiency and Muscle Function: More Than Just Cramps
- Stages of Magnesium Deficiency and What Happens in Each
- How Magnesium Deficiency Affects the Heart and Blood Pressure
- The Connection Between Magnesium and Mental Health
- Digestive Symptoms That Could Be Magnesium-Related
- Groups Most at Risk for Magnesium Deficiency
- Diagnosing Magnesium Deficiency: Why It’s Hard to Catch
- How to Replenish Magnesium Safely and Effectively
- Natural Ways to Support Magnesium Absorption
- Long-Term Consequences of Ignoring Magnesium Deficiency
- FAQ
What Is Magnesium and Why Your Body Depends on It
Magnesium is a vital mineral that quietly powers more than 300 biochemical processes in your body. From muscle contractions and nerve signals to heartbeat regulation and blood sugar control, magnesium plays a behind-the-scenes role in nearly every major system. But despite its importance, many people have suboptimal levels—often without realizing it.
Modern diets, stress, and certain medications can all interfere with magnesium absorption or increase its loss through urine. And unlike calcium or iron, magnesium doesn’t get much attention until symptoms appear. The problem is, those symptoms often mimic other conditions, making magnesium deficiency a silent disruptor of health.
Understanding magnesium’s role is the first step toward recognizing its impact. When your body doesn’t get enough, it sends warning signs—sometimes subtle, sometimes severe—long before full-blown deficiency occurs.
Early Warning Signs of Magnesium Deficiency
Magnesium deficiency doesn’t usually hit all at once. It builds gradually, and early symptoms can be so subtle that they’re easy to ignore or misattribute. One of the first red flags is often muscle twitches, especially around the eyes or calves. These involuntary spasms happen because magnesium helps regulate nerve impulses—and when levels drop, nerves misfire more easily.
Another early sign is fatigue, even after a full night’s sleep. Without magnesium, your cells struggle to produce energy efficiently, leaving you feeling drained. You might also notice irritability, poor stress tolerance, or mild insomnia.
Some people develop headaches or sensitivity to noise or light. These neurological signs hint that magnesium’s role in calming the nervous system is being disrupted. If ignored, these symptoms can progress into more serious stages that affect your cardiovascular, muscular, and mental health.
Advanced Symptoms of Prolonged Deficiency
As magnesium levels fall further, the symptoms intensify and affect more critical systems in the body. Muscle cramps and spasms become more frequent and painful—especially at night. You may also notice tingling or numbness in the hands, feet, or face, as nerve function declines.
More concerning are heart palpitations, irregular heartbeat, or even chest tightness. Magnesium helps regulate electrical activity in the heart, and deficiency can destabilize this rhythm. Some individuals also experience high blood pressure, as magnesium works to relax blood vessels and keep pressure in check.
On the mental health side, symptoms can escalate into anxiety, panic attacks, or persistent depression. Magnesium supports serotonin production, and low levels are directly linked to mood disorders. These deeper symptoms are signs that deficiency has reached a critical stage and must be addressed urgently.
Physical, Emotional, and Neurological Symptoms Linked to Low Magnesium
Magnesium deficiency doesn’t affect just one part of your body—it has wide-reaching effects. Here’s how it manifests across physical, mental, and neurological systems:
Physical symptoms often include muscle weakness, tremors, fatigue, poor coordination, or constipation. Some people also report jaw clenching or teeth grinding, particularly at night.
Emotional symptoms might show up as mood swings, increased sensitivity to stress, or a feeling of restlessness that’s hard to shake. You may feel easily overwhelmed or experience a “wired but tired” sensation that disrupts sleep.
Neurological symptoms include memory problems, brain fog, confusion, difficulty concentrating, and in extreme cases, seizures. Since magnesium helps regulate neurotransmitters, a deficiency can deeply disturb how the brain processes signals and emotions.
Recognizing this wide symptom spread is crucial—especially if multiple symptoms show up at the same time. Often, magnesium deficiency is hiding in plain sight, disguised as something else.

Hidden Causes of Magnesium Deficiency You Might Not Notice
It’s not just poor diet that causes magnesium levels to drop. There are several hidden factors that deplete magnesium, often without warning. One major contributor is chronic stress. When you’re under stress, your body uses more magnesium to support the nervous system, and your levels drop faster than usual.
Certain medications—such as proton pump inhibitors (for acid reflux), diuretics, and some antibiotics—can either block magnesium absorption or increase urinary loss. Even birth control pills and hormone replacement therapy can play a role over time.
Digestive disorders, like Crohn’s disease, IBS, or celiac disease, also impair absorption by damaging the gut lining. So even if your diet includes magnesium-rich foods, your body may not be absorbing enough. Alcohol consumption, especially when habitual, drains magnesium stores rapidly and interferes with vitamin D, which is needed for proper magnesium balance.
If these factors apply to you, magnesium deficiency may already be at play—even if you haven’t yet connected the dots.
How Magnesium Deficiency Affects Sleep Quality
If you struggle with insomnia, frequent waking, or unrefreshing sleep, magnesium might be the missing link. This mineral is vital for calming the nervous system and helping the brain produce GABA, a neurotransmitter that promotes deep, restorative sleep.
People with low magnesium often describe being “tired but wired”—mentally exhausted yet physically restless. They may lie awake for hours or wake frequently in the early morning hours without being able to fall back asleep. Magnesium also helps regulate melatonin production, the hormone responsible for the sleep-wake cycle.
Correcting a magnesium deficiency has been shown to improve sleep latency (how long it takes to fall asleep), reduce nighttime awakenings, and enhance sleep depth. For many people, sleep is the first thing that noticeably improves once magnesium levels are restored.

Magnesium Deficiency and Muscle Function: More Than Just Cramps
While muscle cramps are a well-known symptom, magnesium’s role in muscle health goes much deeper. This mineral is essential for proper muscle relaxation after contraction. Without it, muscles stay tense, leading to stiffness, spasms, and sometimes tremors.
In athletes or active individuals, magnesium deficiency can also cause poor performance, increased risk of injury, and slower recovery. This is because magnesium is involved in ATP production—the energy currency of muscle cells.
People with low magnesium may also experience restless leg syndrome, particularly at night, or a “buzzing” feeling in their limbs. These sensations stem from nerve hyperexcitability and muscular fatigue. Addressing magnesium deficiency helps the body reset these systems, improving both movement and rest.
Stages of Magnesium Deficiency and What Happens in Each
The impact of magnesium deficiency depends on how long it’s been progressing. Here’s a stage-by-stage breakdown:
| Stage | What Happens in the Body | Typical Symptoms |
| Mild deficiency | Body starts drawing magnesium from bones to maintain blood levels | Twitching eyelids, fatigue, mild irritability |
| Moderate deficiency | Blood magnesium drops; nerve and muscle function begin to falter | Muscle cramps, poor sleep, anxiety, frequent headaches |
| Severe deficiency | Systemic dysfunction; major organs and heart may be affected | Irregular heartbeat, numbness, confusion, depression, weakness |
| Chronic deficiency | Long-term depletion affects bones, heart, brain, and digestion | Osteoporosis risk, high blood pressure, cognitive decline, insomnia |
Knowing where you are on this timeline helps determine the urgency of correcting your magnesium intake—and whether lifestyle or medical treatment is needed.
How Magnesium Deficiency Affects the Heart and Blood Pressure
Magnesium is deeply involved in maintaining cardiovascular stability. It regulates electrical signals in the heart, supports blood vessel flexibility, and helps control blood pressure. When magnesium levels drop too low, the heart becomes more susceptible to irregular rhythms, palpitations, and even dangerous arrhythmias.
One common sign is a racing or skipping heartbeat, especially when resting or during periods of stress. Magnesium helps the heart muscle relax between beats, and without it, the rhythm can become erratic. Over time, low magnesium can contribute to high blood pressure, because it prevents the arteries from properly dilating.
This mineral also works alongside calcium and potassium to balance electrolyte levels and maintain smooth muscle tone in the blood vessels. Studies have linked chronic magnesium deficiency to increased risk of heart disease, especially when paired with other factors like poor diet or elevated stress.
The Connection Between Magnesium and Mental Health
Mental health is one of the most overlooked areas affected by magnesium deficiency. This mineral plays a crucial role in regulating neurotransmitters such as serotonin, dopamine, and GABA—all of which influence mood, emotion, and focus.
People with low magnesium often report persistent anxiety, frequent panic attacks, depressive episodes, and even feelings of hopelessness. This isn’t just psychological—magnesium deficiency increases cortisol levels (the stress hormone), while lowering the brain’s natural calming mechanisms.
In some individuals, magnesium deficiency may mimic symptoms of ADHD, including poor concentration, irritability, and impulsivity. Supplementing magnesium has been shown to reduce anxiety and improve mood stability, especially in people who are under chronic stress or recovering from trauma.
The mind and body are deeply connected through magnesium, making it essential for emotional resilience and cognitive clarity.
Digestive Symptoms That Could Be Magnesium-Related
The digestive system both influences and reflects magnesium status. On one hand, low magnesium can cause gastrointestinal issues; on the other, digestive problems can worsen magnesium absorption.
People with low magnesium may experience constipation, due to impaired muscle contractions in the intestines. The mineral is vital for drawing water into the bowel and helping stool move smoothly. Without it, digestion slows and discomfort builds.
Other symptoms can include loss of appetite, nausea, and bloating. In severe cases, vomiting or difficulty swallowing may occur, especially if nerve signaling to the gut is disrupted.
Those with malabsorption conditions—like Crohn’s disease, IBS, or chronic gastritis—are at higher risk of deficiency because the gut lining can’t efficiently absorb nutrients, even when intake is sufficient.
Groups Most at Risk for Magnesium Deficiency
While magnesium deficiency can affect anyone, certain populations are significantly more vulnerable due to lifestyle, health conditions, or age.
- Older adults often absorb less magnesium due to decreased stomach acid and may lose more through medications like diuretics.
- People with diabetes are at higher risk because excess glucose in the kidneys pulls magnesium out with it, leading to urinary loss.
- Athletes can become deficient from heavy sweating, muscle stress, and energy demands, especially without proper recovery nutrition.
- Pregnant women need more magnesium to support fetal development and manage muscle and nerve function, but it’s often overlooked in prenatal care.
- People with high stress levels or poor diets (low in leafy greens, nuts, seeds, and legumes) are also at higher risk due to chronic depletion.
Understanding your risk profile makes it easier to take preventive action before symptoms develop or worsen.
Diagnosing Magnesium Deficiency: Why It’s Hard to Catch
Magnesium deficiency is notoriously underdiagnosed—even by professionals—because most magnesium is stored inside cells and bones, not in the bloodstream. Standard blood tests only measure about 1% of total magnesium in the body, and levels can appear “normal” even when tissues are severely depleted.
Doctors who suspect a deficiency may order a serum magnesium test, but this often misses the mark. A better indicator is the RBC magnesium test, which measures how much magnesium is stored in red blood cells. Some specialists also look at symptoms and risk factors rather than relying on labs alone.
Because of this complexity, many people live with chronic magnesium deficiency for years before getting a diagnosis. If you have multiple symptoms—especially involving muscles, sleep, digestion, or mood—it may be worth exploring magnesium levels with a holistic or functional medicine provider.
How to Replenish Magnesium Safely and Effectively
Restoring magnesium levels can be simple, but it requires consistency. The most sustainable way is through food sources, such as dark leafy greens, pumpkin seeds, almonds, avocados, beans, and whole grains. These foods not only contain magnesium, but also the co-factors (like B vitamins) that support absorption.
For those with moderate to severe deficiency, supplements may be necessary. Common forms include:
- Magnesium glycinate – gentle on digestion and calming to the nervous system
- Magnesium citrate – good for constipation but may cause loose stools
- Magnesium malate – energizing and good for muscle support
- Magnesium threonate – crosses the blood-brain barrier and supports cognitive function
Start low and increase gradually. Many people benefit from 200–400 mg per day, but dosages depend on symptoms, absorption, and existing levels. It’s important to consult a healthcare provider, especially if you have kidney issues or take medication that affects electrolytes.
Natural Ways to Support Magnesium Absorption
Even the best magnesium intake won’t help if your body can’t absorb it. To support absorption, avoid drinking caffeine or alcohol near magnesium-rich meals or supplements, as both can interfere with uptake.
Vitamin D, vitamin B6, and selenium all help shuttle magnesium into cells. Spending time in sunlight or taking D3 supplements may indirectly support magnesium status. Gut health also matters—repairing the digestive tract with probiotics, fermented foods, and anti-inflammatory nutrients like L-glutamine can boost nutrient absorption.
Some people find success using transdermal magnesium, such as sprays, oils, or Epsom salt baths. These bypass digestion and absorb through the skin, offering relief for muscle cramps or tension.
The more supportive your overall environment is, the easier it becomes for your body to retain and use magnesium properly.
Long-Term Consequences of Ignoring Magnesium Deficiency
When magnesium deficiency goes untreated, it can quietly erode your health over months or years. Persistent low levels have been linked to osteoporosis, chronic fatigue syndrome, high blood pressure, migraines, type 2 diabetes, and cardiovascular disease.
Because magnesium interacts with calcium, potassium, and vitamin D, deficiencies can cause systemic imbalances that lead to bone loss, nerve damage, or arrhythmias. Even mood disorders like depression and anxiety may become chronic when low magnesium is involved.
Over time, your body loses its resilience to physical and emotional stress, healing slows down, and inflammation becomes harder to control. The good news? Replenishing magnesium—even after years of deficiency—often brings surprising improvements in sleep, focus, pain, and energy.
Prevention is far easier than recovery, and maintaining healthy magnesium levels is one of the simplest yet most powerful things you can do for your overall well-being.
FAQ
What are the earliest signs of magnesium deficiency?
The earliest signs are often subtle and include muscle twitches, especially around the eyelids or calves, as well as fatigue, mild anxiety, and trouble sleeping. Some people also experience occasional headaches or increased sensitivity to noise. These symptoms are usually the body’s quiet signal that magnesium stores are running low—even if blood tests still appear normal.
Why is magnesium deficiency so common today?
Modern lifestyles and diets contribute heavily. Processed foods are stripped of minerals, and chronic stress depletes magnesium rapidly. On top of that, medications like antacids, diuretics, and some antibiotics interfere with absorption. Even healthy eaters may be deficient due to poor soil quality, digestive issues, or high stress levels.
Can magnesium deficiency cause anxiety or panic attacks?
Yes, magnesium is directly involved in regulating the nervous system and producing calming neurotransmitters like GABA. When levels drop, the brain becomes more reactive, and people may feel anxious, overstimulated, or even panicky—especially during stressful events. Supplementing with magnesium often leads to noticeable improvements in mood stability.
How do I know if my magnesium levels are low?
Unfortunately, standard blood tests may not reveal the problem since they only measure 1% of magnesium found in the blood. Symptoms are often the clearest indicators. If you experience frequent muscle cramps, fatigue, irritability, poor sleep, or digestive issues, it may be worth requesting an RBC magnesium test or consulting a functional health provider.
Can magnesium deficiency cause heart palpitations?
Yes, magnesium is essential for maintaining normal electrical rhythm in the heart. Low levels can lead to palpitations, fluttering, or even irregular heartbeat. This is especially concerning if paired with other symptoms like chest tightness or dizziness. Replenishing magnesium can often help stabilize the rhythm—especially when paired with potassium and hydration.
Is low magnesium linked to poor sleep?
Absolutely. Magnesium helps regulate melatonin and GABA, both essential for initiating and maintaining restful sleep. Deficiency can lead to trouble falling asleep, frequent waking, or feeling unrefreshed in the morning. Many people report much deeper and more restorative sleep once they correct low magnesium levels.
Can magnesium deficiency cause numbness or tingling?
Yes, prolonged deficiency can affect nerve conduction, leading to tingling, numbness, or a “pins and needles” feeling—usually in the hands, feet, or face. This symptom often mimics conditions like B12 deficiency or peripheral neuropathy, but magnesium is a key player in healthy nerve signaling as well.
Are headaches and migraines related to low magnesium?
They can be. Magnesium helps regulate blood vessel tone in the brain, and deficiency may trigger vascular constriction and inflammation—leading to headaches or migraines. Many neurologists recommend magnesium as part of a prevention strategy for people with chronic migraines, especially when other symptoms of deficiency are present.
Which foods are high in magnesium?
Natural sources include pumpkin seeds, almonds, spinach, black beans, avocados, whole grains, dark chocolate, and tofu. The body absorbs magnesium from food more steadily than from supplements, so increasing dietary intake is the best first step to long-term balance.
What’s the best form of magnesium to take?
That depends on your symptoms. Magnesium glycinate is gentle on digestion and great for anxiety and sleep. Magnesium citrate is more laxative and helpful for constipation. Magnesium malate supports energy and muscles, while magnesium threonate targets the brain and may help with focus or memory. Avoid magnesium oxide—it’s poorly absorbed.
Can I take too much magnesium?
Yes, though the risk is low if you’re healthy. Too much supplemental magnesium—especially from poorly absorbed forms like magnesium oxide—can cause diarrhea, nausea, or abdominal cramping. People with kidney disease should be especially cautious, as they can’t excrete excess magnesium efficiently. Always start low and adjust based on response.
How long does it take to correct a magnesium deficiency?
Most people begin to notice improvements within 1–3 weeks of consistent supplementation or dietary changes. However, full restoration of magnesium stores—especially after prolonged deficiency—may take 1–3 months or longer. Patience and regular intake are key to long-term success.
Is transdermal magnesium (spray or bath) effective?
Yes, many people find magnesium oil sprays or Epsom salt baths helpful, especially for muscle cramps or nighttime leg discomfort. While absorption through the skin may vary, these methods bypass the digestive system and provide localized relief. They’re ideal for those with sensitive stomachs or trouble absorbing magnesium orally.
Does magnesium interact with any medications?
Yes. Magnesium can interfere with the absorption of antibiotics, thyroid medication, and bisphosphonates (used for bone health). It also amplifies the effect of some blood pressure meds. Always take magnesium supplements at least 2 hours apart from prescription drugs, and consult your healthcare provider if you’re unsure.
Can children or teens be deficient in magnesium?
Yes, especially those with restricted diets, chronic stress, high sugar intake, or digestive disorders. Kids with ADHD or behavioral issues may also show signs of low magnesium. Supplementing—under pediatric supervision—has been shown to improve focus, mood, and sleep in some cases.










