Blood Tests for Lymphomas: An In-Depth Clinical Guide
While no single blood test can definitively diagnose lymphoma, bloodwork plays a crucial supporting role in identifying red flags, staging the disease, and monitoring treatment response. As an oncologist, I regularly see cases where the first sign of lymphoma was a subtle shift in blood values, long before the diagnosis was confirmed through imaging or biopsy.
This guide explains what to expect from your bloodwork if lymphoma is suspected — and just as importantly, what normal results do not rule out.
Lymphoma with Normal CBC Test Results
It surprises many patients to learn that a completely normal complete blood count (CBC) does not exclude lymphoma. In fact, early-stage lymphomas — particularly Hodgkin’s lymphoma — may leave blood counts untouched for months.
Why can the CBC be normal in lymphoma?
Lymphomas originate in the lymphatic system, not the bone marrow. Unless the cancer has spread to the marrow or triggered systemic inflammation, standard blood counts like WBC, RBC, or platelets may remain in the normal range.
However, some indirect clues can be present:
- Mild lymphocytosis or lymphopenia
- Slight anemia (normocytic, normochromic)
- Elevated neutrophils (if there’s secondary infection)
- Eosinophilia (in rare subtypes)
What this means for diagnosis
A normal CBC cannot be used to rule out lymphoma. It should always be interpreted in the context of symptoms and imaging. If lymphoma is still suspected, further evaluation is mandatory.
| CBC Parameter | Possible Change in Lymphoma | Interpretation |
|---|---|---|
| Hemoglobin | Often normal or mildly low | Anemia of chronic disease in later stages |
| WBC | Normal, low, or high | Non-specific; depends on subtype |
| Platelets | Normal or low | May drop in marrow involvement |
| Lymphocytes | Low in Hodgkin’s, high in some NHL | Useful trend but not diagnostic |
Lymphoma Blood Test Normal Range
When reviewing blood test results in suspected lymphoma, understanding “normal” ranges is important — but context is key. Many lymphoma cases present with bloodwork within standard limits, particularly early on.
Below is a reference of normal ranges, compared to possible trends in lymphoma:
| Test | Normal Range | Common Changes in Lymphoma |
|---|---|---|
| Hemoglobin | 13.5–17.5 g/dL (men) / 12.0–15.5 g/dL (women) | ↓ in advanced disease |
| WBC | 4,000–11,000 /μL | Normal, ↑ or ↓ depending on subtype |
| Lymphocytes | 1,000–4,800 /μL | ↓ in Hodgkin’s, ↑ in CLL/NHL |
| Platelets | 150,000–450,000 /μL | May decrease in marrow infiltration |
| LDH | < 250 U/L | ↑ in aggressive lymphomas |
| ESR | < 20 mm/hr | Often elevated |
| CRP | < 5 mg/L | Often elevated |
Notes:
- Elevated LDH and ESR are often the most telling biochemical abnormalities in lymphoma — signaling cell turnover and inflammation.
- A normal CBC but elevated LDH should raise suspicion, especially with systemic symptoms (fever, night sweats, weight loss).
Hodgkin’s Lymphoma Blood Test Markers
Hodgkin’s lymphoma (HL) has unique biological and clinical features, and while blood tests cannot confirm the diagnosis, they often show distinct patterns.
Common blood markers seen in Hodgkin’s lymphoma:
- Lymphopenia — paradoxical low lymphocyte count is common, despite HL being a cancer of lymphoid cells.
- Elevated ESR — erythrocyte sedimentation rate is often significantly raised, especially in active or bulky disease.
- Mild normocytic anemia — common due to chronic inflammation or bone marrow suppression.
- Increased LDH — reflects high cellular turnover, often associated with poorer prognosis.
- Hypoalbuminemia — due to systemic inflammation and cytokine release.
- Leukocytosis or eosinophilia — in some patients, white count or eosinophils may be elevated, especially in advanced stages.
| Marker | Typical Range | Hodgkin’s Pattern |
|---|---|---|
| Lymphocytes | 1.0–4.8 ×10⁹/L | Often ↓ |
| ESR | <20 mm/hr | Often >50 mm/hr |
| LDH | <250 U/L | Mild to moderate ↑ |
| CRP | <5 mg/L | Elevated |
| Albumin | 35–50 g/L | ↓ in systemic disease |
Summary
No single test diagnoses HL. The combination of lymphopenia, elevated ESR/CRP, and systemic symptoms should trigger imaging and biopsy. These labs are also used to stage and monitor treatment response over time.
Non-Hodgkin’s Lymphoma Diagnosis Blood Test
Non-Hodgkin’s lymphoma (NHL) includes over 60 subtypes, ranging from slow-growing (indolent) to aggressive forms. Blood test findings vary significantly depending on the grade, subtype, and extent of disease.
Key patterns in NHL:
- Elevated LDH — particularly in diffuse large B-cell lymphoma (DLBCL) or Burkitt lymphoma.
- Elevated beta-2 microglobulin — a tumor burden marker useful in CLL and follicular lymphoma.
- Lymphocytosis — seen in leukemic variants like CLL or SLL.
- Cytopenias — occur when the bone marrow is infiltrated.
Useful blood tests in NHL diagnosis:
| Test | Role |
|---|---|
| CBC with differential | Detects cytopenias or lymphocytosis |
| LDH | Tumor burden indicator |
| Beta-2 microglobulin | Prognostic marker |
| Serum protein electrophoresis | Detects monoclonal gammopathy (e.g., Waldenström’s) |
| Flow cytometry (peripheral blood) | Essential for leukemic NHL subtypes |
| HIV/Hep C screening | Required before treatment (due to reactivation risk) |
While blood tests can suggest NHL, definitive diagnosis requires a lymph node biopsy. However, in leukemic forms like CLL, diagnosis can sometimes be made entirely via blood and flow cytometry.
How Long Does It Take to Diagnose Lymphoma?
The timeline for diagnosing lymphoma varies depending on the initial presentation and availability of tests, but the process often takes 7 to 21 days.
Typical diagnostic steps and timeframe:
- Initial bloodwork: 1–2 days
- Imaging (CT or PET scan): 2–5 days after referral
- Lymph node biopsy: Scheduled within 3–7 days
- Histopathology + Immunohistochemistry: 5–10 days after biopsy
- Bone marrow biopsy (if needed): adds 2–3 days
- Staging + treatment planning: 2–5 days after full workup
| Step | Approx. Time |
|---|---|
| Primary care to referral | 2–5 days |
| Diagnosis to staging | 7–10 days |
| Total from suspicion to confirmed subtype | ~2–3 weeks |
Factors that may delay diagnosis:
- Deep or inaccessible lymph nodes (requiring surgical biopsy)
- Atypical presentations (e.g., normal imaging or labs)
- Indolent subtypes without clear symptoms
Despite these variables, most cancer centers aim to initiate treatment within 21–28 days of initial suspicion.
Symptoms of Lymphoma in Females
Lymphoma symptoms in females are largely the same as in males, but hormonal factors, reproductive physiology, and delayed recognition can modulate presentation and progression.
General symptoms common in both sexes:
- Persistent fatigue
- Swollen lymph nodes (especially in neck, armpits, groin)
- Unexplained weight loss
- Fever without infection
- Night sweats
- Itching or skin rashes
- Shortness of breath or cough (from mediastinal nodes)
Specific considerations in women:
- Misattribution to menstrual or hormonal cycles: Fatigue, bloating, or night sweats may be overlooked as perimenopausal or hormonal.
- Pelvic or ovarian lymphomas: May mimic gynecological conditions such as fibroids or cysts.
- Breast involvement (primary breast lymphoma): Rare but important, presenting as a painless breast mass.
When women should seek evaluation:
- Swollen lymph nodes lasting >2 weeks
- Persistent fatigue unrelieved by rest
- Night sweats soaking sheets
- Post-menopausal bleeding + lymphadenopathy
- Unexplained pruritus (itching) without rash
| Symptom | Relevance in Females |
|---|---|
| Night sweats | May be dismissed as hormonal |
| Pelvic discomfort | Possible extranodal disease |
| Breast lump | Consider lymphoma if non-typical imaging |
| Abdominal swelling | May mimic ovarian mass |
How Is Lymphoma Diagnosed
Lymphoma diagnosis is a multistep, multidisciplinary process, requiring integration of clinical, radiologic, histologic, and immunologic findings.
Step 1: Clinical suspicion
Raised when a patient presents with enlarged lymph nodes, systemic symptoms (fever, night sweats, weight loss), or unexplained lab abnormalities.
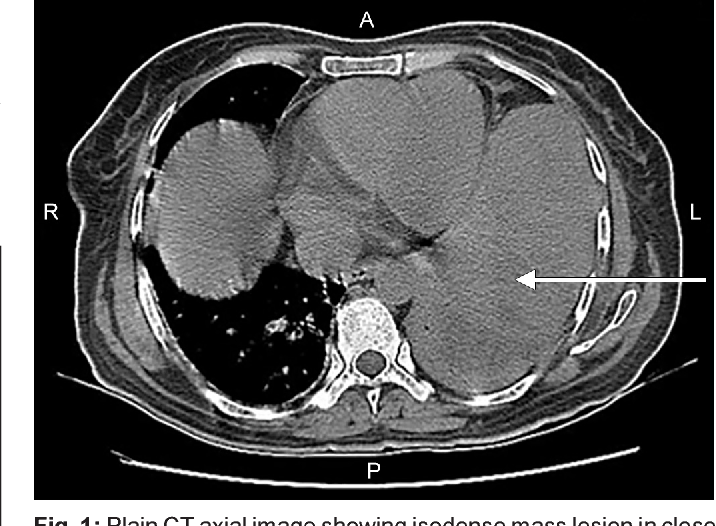
Step 2: Imaging
- CT scan: First-line for identifying lymph node clusters
- PET-CT: Assesses metabolic activity and helps in staging
- Ultrasound: Useful for superficial nodes
Step 3: Biopsy
- Excisional biopsy (gold standard): Entire lymph node removed
- Core needle biopsy: Used if excision not possible
- Bone marrow biopsy: Done in most advanced or high-grade cases
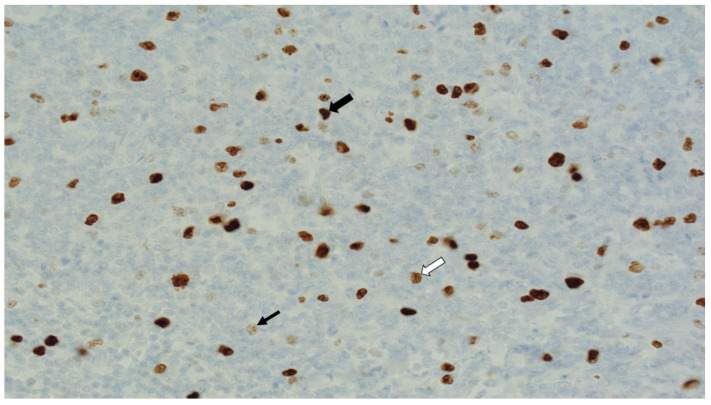
Step 4: Histopathology + Immunophenotyping
- CD20, CD3, CD30, Ki-67, etc. determine B-cell or T-cell lineage and grade
- Flow cytometry, FISH, and cytogenetics refine the diagnosis
| Diagnostic Tool | Purpose |
|---|---|
| Lymph node biopsy | Confirm malignancy and type |
| PET/CT | Stage the disease |
| Bone marrow biopsy | Detect marrow involvement |
| Flow cytometry | Immunophenotypic profile |
| Bloodwork (LDH, CBC) | General tumor activity |
Takeaway
Only a biopsy confirms lymphoma. Blood tests and imaging guide suspicion, but no diagnosis can be made without histologic evidence.
How Bad Is Lymphoma Cancer?
Lymphoma is a very heterogeneous disease — ranging from indolent forms that don’t need immediate treatment to aggressive subtypes that require urgent chemotherapy.
Favorable prognosis (highly treatable):
- Hodgkin’s lymphoma (especially early-stage)
- Diffuse large B-cell lymphoma (DLBCL) when diagnosed early
- Burkitt lymphoma, though aggressive, responds well to intensive therapy
Indolent but chronic:
- Follicular lymphoma
- Chronic lymphocytic leukemia (CLL)
These often relapse multiple times but can be managed long-term.
Poorer prognosis:
- T-cell lymphomas
- Double/triple hit lymphomas (with MYC, BCL2, BCL6 mutations)
- Relapsed/refractory cases or disease with CNS involvement
| Subtype | Typical Outlook |
|---|---|
| Hodgkin’s lymphoma | ~90% 5-year survival (early) |
| DLBCL | 60–80% cure rate (first-line) |
| Follicular lymphoma | Median survival ~15 years |
| Peripheral T-cell lymphoma | Less than 30% long-term survival |
| Burkitt lymphoma | ~75–85% survival in young adults |
Final thoughts
Lymphoma is very treatable in most cases, especially when diagnosed early. Prognosis depends on subtype, stage, age, performance status, and genetic markers. Even aggressive types can be cured with timely treatment.
Blood Tests for Lymphomas – FAQ
Can lymphoma show up in blood tests?
Not directly. Lymphoma is diagnosed via biopsy, but blood tests can reveal red flags like elevated LDH, low lymphocytes, or anemia.
Can lymphoma be present with a normal CBC?
Yes. Many lymphomas — especially early-stage — present with a completely normal complete blood count.
What are common blood abnormalities in lymphoma?
Elevated LDH, ESR, or CRP; anemia; low lymphocytes (Hodgkin’s); high lymphocytes (CLL); low platelets (advanced stages).
What is the normal range for lymphoma blood tests?
There is no “lymphoma-specific” blood test. CBC, LDH, ESR, and CRP should be interpreted contextually — often within normal range early on.
What are the blood markers for Hodgkin’s lymphoma?
Common markers include low lymphocytes, high ESR/CRP, elevated LDH, and mild anemia. None are diagnostic alone.
How is non-Hodgkin’s lymphoma diagnosed through blood?
It’s not — diagnosis requires a biopsy. But flow cytometry on blood can confirm leukemic forms like CLL or SLL.
How long does it take to diagnose lymphoma?
Typically 1–3 weeks. It involves imaging, biopsy, pathology, and staging scans.
What are symptoms of lymphoma in females?
Same as in males: fatigue, night sweats, swollen lymph nodes. Some women may have pelvic or breast involvement misinterpreted as gynecological disease.
How serious is lymphoma?
It depends on the subtype. Hodgkin’s and many B-cell lymphomas are highly treatable. Some T-cell or aggressive forms are harder to cure.
Can lymphoma be detected in routine bloodwork?
Sometimes. Persistent elevation of LDH, unexplained anemia, or abnormal lymphocyte counts should raise suspicion — but biopsy is essential for diagnosis.
Does high LDH always mean lymphoma?
No. LDH can rise in infections, hemolysis, and other cancers. But in lymphoma, it’s a marker of aggressive disease and tumor burden.
Can you have lymphoma without swollen lymph nodes?
Yes. Some extranodal lymphomas affect the GI tract, brain, or bone marrow without noticeable lymphadenopathy.
Are blood tests enough to rule out lymphoma?
No. Normal blood tests don’t exclude lymphoma. Imaging and biopsy are always needed if symptoms persist.
What is beta-2 microglobulin used for?
It’s a tumor burden marker in lymphomas like CLL, myeloma, and follicular lymphoma — higher levels often indicate more advanced disease.
What imaging is used for lymphoma diagnosis?
CT and PET-CT scans are standard for staging and evaluating disease activity.