What Type of Cancer Causes Low Hemoglobin (Anemia)?
Low hemoglobin, or anemia, is a common issue in cancer patients. It may result from the cancer itself, its treatment, or underlying nutritional deficiencies. As an oncologist, I often encounter patients where anemia is the first clinical clue of an undiagnosed malignancy. In this article, we’ll explore what types of cancer are most likely to cause low hemoglobin, how anemia relates to cancer outcomes, and what it may signal.
Cancers That Cause Anemia
Anemia is not exclusive to cancer. However, certain malignancies are particularly prone to lowering hemoglobin levels due to bone marrow infiltration, chronic bleeding, or systemic inflammation.
Blood and Bone Marrow Cancers
Cancers such as leukemia, lymphoma, and multiple myeloma directly interfere with the production of red blood cells. In these conditions, malignant cells replace normal hematopoietic cells, leading to decreased production of hemoglobin and other blood components.
How serious is myeloma cancer?
Multiple myeloma is a serious and chronic cancer of plasma cells. It often presents with anemia, bone pain, and kidney dysfunction. While it is not curable, it is treatable, and outcomes vary based on stage and response to therapy.
Cervical Cancer
Cervical cancer can cause chronic vaginal bleeding, especially in advanced stages, leading to gradual but significant iron-deficiency anemia. In many cases, women may first present with fatigue or weakness before the cancer is detected.
Colon Cancer
What type of cancer causes low hemoglobin?
Colon cancer is one of the most common malignancies linked to low hemoglobin, particularly when tumors bleed slowly into the gastrointestinal tract. This may occur without visible signs of blood loss, making anemia a key diagnostic clue.
Kidney Cancer
The kidneys regulate erythropoietin (EPO), the hormone that stimulates red blood cell production. Kidney tumors may suppress EPO, leading to normocytic anemia. In rare cases, tumors may overproduce EPO, resulting in high hemoglobin levels instead.
High hemoglobin cancer
While most cancers cause low hemoglobin, a few — particularly renal cell carcinoma and hepatic tumors — can lead to polycythemia (elevated red cell count) due to ectopic EPO production.
Breast Cancer
Breast cancer rarely causes anemia on its own, but advanced disease and chemotherapy often lead to lowered hemoglobin due to marrow suppression, nutritional depletion, or inflammation.
Ferritin, Anemia, and Cancer
Ferritin is a protein that stores iron. In cancer, ferritin may paradoxically be elevated, not because of iron abundance, but due to inflammation (as an acute phase reactant). This can mask true iron deficiency and complicate anemia management.
Prostate Cancer
Prostate cancer can cause bone marrow metastases, impairing red blood cell production. Hormone therapy, frequently used in advanced cases, also contributes to anemia by altering metabolism and suppressing marrow activity.
Lung Cancer
Can lung cancer cause anemia?
Yes. Lung cancer may cause anemia via several pathways: chronic inflammation, bone marrow involvement, nutritional depletion, or chemotherapy side effects. Anemia is especially common in advanced-stage non-small cell lung cancer (NSCLC).
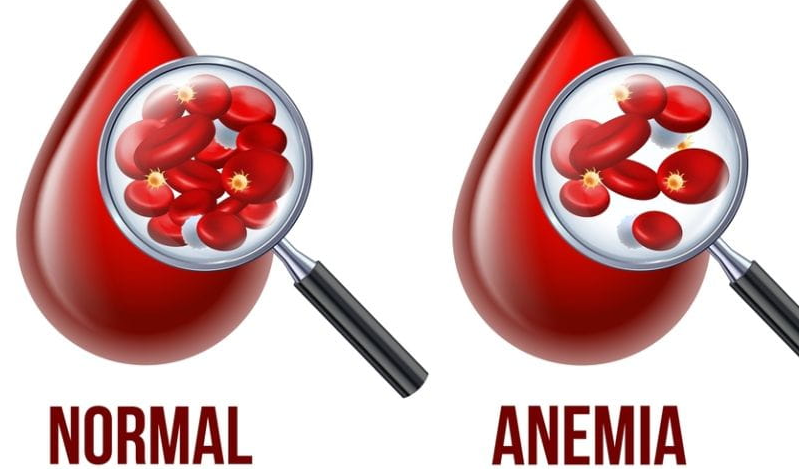
Cancer’s Impact on Red Blood Cells
Cancer affects red blood cell production in three major ways:
- Bone marrow suppression: from infiltration or treatment
- Chronic blood loss: particularly in GI or gynecological cancers
- Inflammation: which inhibits iron use and erythropoietin effectiveness
This triad is known as anemia of chronic disease, a frequent finding in oncology.
Cancer Treatment and Anemia
Chemotherapy, radiation, and immunotherapy can all suppress bone marrow, reducing hemoglobin levels. Treatments that cause myelosuppression (especially platinum-based regimens) are most likely to result in anemia.
Supportive treatments include:
- Erythropoiesis-stimulating agents (ESAs)
- Iron therapy (if deficient)
- Blood transfusions in symptomatic or severe cases
- Addressing underlying bleeding sources
Low Hemoglobin Cancer Symptoms
Patients with cancer-related anemia often report:
- Fatigue
- Shortness of breath
- Pale skin
- Chest discomfort
- Lightheadedness
- Reduced exercise tolerance
These symptoms may be subtle at first, but they progress as hemoglobin drops further.
Anemia Symptoms
When to Seek Emergency Care
Seek immediate medical attention if anemia leads to:
- Chest pain
- Difficulty breathing at rest
- Dizziness with standing or blackouts
- Rapid heart rate or palpitations
These may indicate severe or life-threatening anemia, particularly in patients with underlying cardiac disease.
Diagnosis
Diagnosing Cancer
While anemia can signal cancer, hemoglobin levels alone do not detect cancer. A full diagnostic workup includes:
- CBC (complete blood count)
- Iron studies (ferritin, transferrin saturation)
- Reticulocyte count
- Bone marrow biopsy (if indicated)
- Imaging (CT, PET)
- Colonoscopy, endoscopy (for GI sources)
Does Anemia Mean Cancer?
Not always. Most anemia is non-malignant, caused by iron deficiency, menstruation, kidney disease, or chronic inflammation. However, in older adults or in the presence of unexplained anemia, cancer should always be considered — especially if iron-deficiency is found without a clear source.
Can Hemoglobin Levels Detect Cancer?
Hemoglobin levels alone cannot detect cancer, but:
- Low hemoglobin may trigger further investigation
- Unexplained anemia often leads to discovery of GI, hematologic, or renal tumors
- In cancer patients, hemoglobin trends can monitor disease activity or treatment side effects
What Blood Markers Indicate Cancer?
Beyond hemoglobin, important cancer-related blood markers include:
- LDH — tissue turnover (e.g., lymphoma, melanoma)
- Ferritin — inflammation vs. iron overload
- ESR/CRP — systemic inflammation
- Tumor markers — CEA, CA-125, PSA, CA 19-9, AFP
- White cell count / Platelets — marrow activity and paraneoplastic syndromes
How to Increase Hemoglobin in Cancer Patients
Improving hemoglobin in cancer patients involves:
- Identifying the cause — iron deficiency vs. inflammation vs. marrow suppression
- Iron supplementation — oral or IV depending on tolerance
- Erythropoietin-stimulating agents — used in selected cases (with caution due to thrombotic risk)
- Transfusion support — for acute or severe anemia
- Nutrition optimization — ensuring adequate B12, folate, protein, and calories
- Reducing marrow-toxic therapies — when possible or adjusting doses
Cancer patients hemoglobin levels should ideally be kept above 10 g/dL, though many tolerate slightly lower levels if asymptomatic.
What Percentage of Anemia Is Cancer?
In population studies, 3–10% of unexplained anemia in adults is ultimately linked to an underlying malignancy — most commonly gastrointestinal or hematologic cancers. In patients over 60, especially with iron-deficiency anemia, cancer should always be ruled out.
FAQ: Low Hemoglobin and Cancer
Can low hemoglobin be the first sign of cancer?
Yes. In some patients, unexplained anemia is the very first clinical clue that leads to a cancer diagnosis — especially colon, stomach, or blood-related cancers.
Does anemia always mean cancer?
No. Anemia is common and usually caused by non-cancerous conditions like iron deficiency, menstruation, or kidney disease. But in older adults, it should always be investigated.
What type of cancer causes low hemoglobin most often?
Gastrointestinal cancers (like colon or stomach), blood cancers (like leukemia or myeloma), and kidney cancers are the most common culprits.
Can lung cancer cause anemia?
Yes. Lung cancer can cause anemia through chronic inflammation, bone marrow involvement, or as a side effect of treatment.
Is low hemoglobin in a cancer patient dangerous?
It can be. If hemoglobin drops too low (below ~8 g/dL), it can cause heart strain, fatigue, and reduced treatment tolerance. Severe cases may need transfusion.
What hemoglobin level is considered critical in cancer patients?
Below 7–8 g/dL is typically considered critical and may require transfusion, especially if the patient is symptomatic.
Can high hemoglobin also be a sign of cancer?
Rarely, yes. Some kidney and liver tumors overproduce erythropoietin, leading to abnormally high red blood cell counts.
How is cancer-related anemia diagnosed?
Through a combination of blood tests (CBC, ferritin, iron, reticulocyte count) and imaging. Sometimes bone marrow biopsy is needed.
What’s the difference between iron-deficiency anemia and cancer-related anemia?
Iron-deficiency is usually from blood loss or poor intake. Cancer-related anemia often stems from inflammation or bone marrow suppression, and ferritin levels may be high despite anemia.
Can chemotherapy cause low hemoglobin?
Yes. Chemotherapy often suppresses bone marrow, reducing red blood cell production and leading to anemia.
Should I take iron supplements if I have cancer and anemia?
Only if you’re iron-deficient. Inflammatory or marrow-related anemia may not respond to iron, and unnecessary supplementation can be harmful.
How can hemoglobin be raised in cancer patients?
Options include treating the underlying cause, using iron (if deficient), erythropoietin injections, transfusions, and nutritional support.
What foods help increase hemoglobin during cancer?
Iron-rich foods (red meat, spinach, lentils), vitamin C (which enhances absorption), B12, and folate are essential — but may not work alone in cancer-related anemia.
Is low hemoglobin a sign that cancer is progressing?
Sometimes. A falling hemoglobin in stable cancer may indicate hidden bleeding, bone marrow involvement, or treatment toxicity.
Is anemia common in breast or prostate cancer?
Yes, especially in advanced stages or during hormone or chemotherapy. It may not be from the tumor itself, but from treatment effects.
Can low hemoglobin delay cancer treatment?
Yes. Severely low levels may lead to dose reductions or treatment delays, as patients won’t tolerate therapy well with oxygen-carrying capacity so reduced.
How often should hemoglobin be checked during cancer treatment?
Usually before each chemotherapy cycle, or every few weeks during active treatment.
Can iron infusions help in cancer-related anemia?
Yes — especially in patients who are iron-deficient and can’t absorb iron orally. They’re often more effective than pills.
What percentage of people with anemia turn out to have cancer?
Roughly 3–10% of adults with unexplained anemia may be diagnosed with cancer, particularly those over age 60.
Can low hemoglobin cause shortness of breath in cancer patients?
Absolutely. Reduced red blood cells mean less oxygen delivery to tissues, leading to fatigue, shortness of breath, and exercise intolerance.