Natural Remedies for Acid Reflux During Pregnancy: Gentle Solutions That Really Work
- What Is Acid Reflux and Why It Happens in Pregnancy
- Early Signs and Symptoms of Reflux in Pregnant Women
- Stages of Acid Reflux in Pregnancy
- The Risks of Ignoring Acid Reflux While Pregnant
- Soothing Foods That Naturally Ease Reflux
- Finding Relief Through Sleep Position and Body Posture
- The Role of Stress in Digestive Discomfort During Pregnancy
- Gentle Eating Habits That Protect Your Digestive Tract
- What to Avoid When Managing Pregnancy Reflux
- Morning Habits That Set the Tone for Better Digestion
- When Natural Approaches May No Longer Be Enough
- The Emotional Power of Support: Partners, Family, and Rest
- Every Body Reacts Differently — and That’s Okay
- Natural Supplements That May Offer Relief
- Evening Rituals for Better Sleep Without Heartburn
- What to Expect After Giving Birth
- FAQ – Natural Relief for Acid Reflux During Pregnancy

What Is Acid Reflux and Why It Happens in Pregnancy
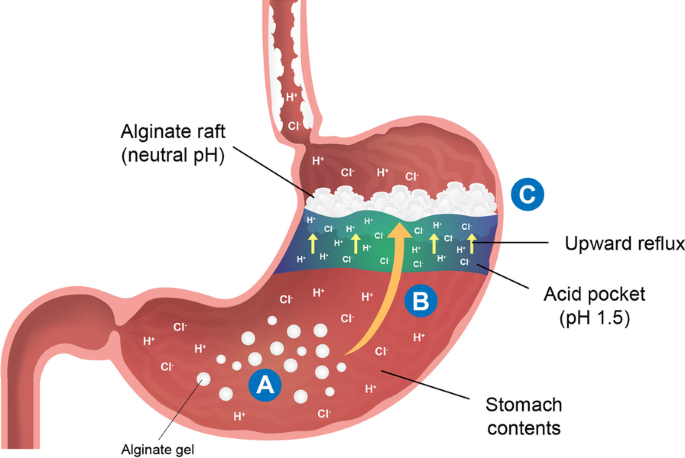
Acid reflux — or gastroesophageal reflux — occurs when stomach acid flows upward into the esophagus. During pregnancy, this issue becomes more frequent due to the hormonal and physical changes taking place.
One of the main culprits is progesterone, a hormone that relaxes muscles — including the lower esophageal sphincter. When this valve weakens, acid has an easier time escaping the stomach. At the same time, as the uterus grows, it pushes up against the stomach, adding pressure that can force acid upward.
I’ve seen this happen in every trimester, but especially in the second and third, when the uterus is expanding rapidly. Reflux can affect sleep, appetite, and even hydration if it becomes too severe.
Early Signs and Symptoms of Reflux in Pregnant Women
It doesn’t always start as dramatic heartburn. Some of the earliest signs are much subtler — and that’s why many women miss them. Based on what I’ve seen over the years, these are the most telling early symptoms:
- A sour taste in the mouth after eating
- Slight burning behind the breastbone after certain foods
- Burping more than usual
- Mild nausea not tied to morning sickness
- Throat irritation or the sensation of something “stuck”
As pregnancy progresses, these signs tend to intensify. Some women describe it as a “slow burn” that turns into full-on discomfort, especially when lying down at night.
Stages of Acid Reflux in Pregnancy
| Stage | Symptoms | What’s Happening in the Body | Risk Level |
| Mild | Occasional sour taste, burping, mild heartburn | Hormonal relaxation of the esophageal sphincter | Low, manageable |
| Moderate | Frequent heartburn, worse after meals or at night | Increased uterine pressure on the stomach | Medium, affects sleep |
| Severe | Persistent burning, trouble swallowing, coughing | Reflux damaging esophageal lining | High, needs treatment |
Understanding where you fall on this spectrum is key to choosing the right natural remedy — some approaches work better in early stages, others are needed for more persistent symptoms.

The Risks of Ignoring Acid Reflux While Pregnant
Many women try to “power through” reflux without treatment, thinking it’s just a normal part of pregnancy. And while it’s true that reflux is common, that doesn’t mean it should be ignored.
Left unchecked, acid reflux can lead to:
- Inflammation of the esophagus (esophagitis)
- Difficulty eating and drinking enough — which can affect fetal nutrition
- Sleep disruptions, which increase pregnancy fatigue
- Coughing and throat irritation, which worsen over time
In some cases, I’ve seen untreated reflux contribute to dehydration or even weight loss. While that’s rare, it’s a clear sign that your body is asking for support. Natural solutions can prevent the condition from escalating — without the side effects of pharmaceuticals.
Soothing Foods That Naturally Ease Reflux
Over the years, I’ve noticed that some foods truly work like a balm for acid reflux — especially during pregnancy when the digestive system is extra sensitive. One thing I always suggest is turning to gentle, cooling options. For instance, warm oatmeal with a little almond milk has brought almost immediate relief to many of my clients. The fiber helps calm digestion, while its texture is easy on the stomach.
Another go-to in my experience is ripe bananas. They’re not only filling and portable, but they seem to create a protective layer in the stomach, which can reduce that uncomfortable burn. I’ve also seen great results with cold, cooked sweet potatoes — simple, nourishing, and surprisingly soothing. Ginger tea, sipped slowly between meals, often helps reduce the sensation of rising acid and settles the stomach without stimulating it.
When I work with someone battling reflux during pregnancy, I often encourage her to rediscover bland but comforting foods — think soft rice, boiled carrots, or a bit of plain yogurt if dairy sits well. While there’s no one-size-fits-all diet, these gentle, real-food options tend to calm inflammation and support digestion in a way that medicine rarely can.
Finding Relief Through Sleep Position and Body Posture
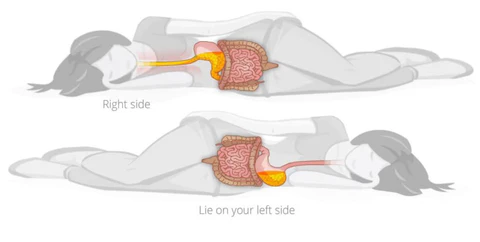
One of the most overlooked factors in managing pregnancy reflux is how you position your body, especially during rest. I’ve seen dramatic improvements when women simply adjust how they lie down. Gravity can either work with you or against you — and during pregnancy, a small change can make a big difference.
When lying flat after meals, acid tends to creep upward into the esophagus. That’s why I always suggest propping up the upper body during rest. You don’t need a fancy pillow system — even placing a few folded towels under the mattress at the head of the bed can raise your angle enough to prevent reflux from rising.
Also, sleeping on your left side seems to be naturally protective. It aligns the stomach in a way that keeps acid lower in the digestive tract. I’ve had clients who made this one simple shift and noticed fewer nighttime flare-ups almost immediately.
Even daytime posture matters. After eating, staying upright — instead of slumping on a couch — allows your stomach to do its job without pressure. Sitting tall at the table or taking a gentle walk after meals can create just enough downward flow to help digestion without triggering reflux.
The Role of Stress in Digestive Discomfort During Pregnancy
What many people don’t realize is how deeply connected stress and digestion are — and during pregnancy, that connection is magnified. I’ve worked with expectant mothers who didn’t feel physically overburdened by what they ate, but emotionally, their bodies were on high alert. And that tension alone was enough to bring on persistent reflux.
When we’re stressed, the body enters a state that diverts blood away from the digestive system. This can slow down stomach emptying and increase pressure — the perfect storm for acid to back up. I’ve also noticed that anxious breathing patterns and clenched posture play a role, further increasing tightness in the diaphragm and esophageal area.
What helped many of my clients wasn’t just dietary change, but learning to exhale deeply before meals, setting their fork down between bites, and even creating a calm, quiet eating space. Some women found relief through prenatal yoga or even just soaking their feet in warm water while listening to soft music in the evening. These rituals might seem small, but when practiced regularly, they tell the body: you’re safe — you can digest now.
Gentle Eating Habits That Protect Your Digestive Tract
Food itself is important, but how you eat it can be just as impactful — especially during pregnancy. I’ve had clients who ate mostly reflux-friendly foods but still struggled, simply because of how quickly or mindlessly they consumed meals.
Rushed eating sends the wrong signals to your gut. When the body isn’t relaxed, it doesn’t secrete digestive enzymes properly. Chewing thoroughly — really giving food time to mix with saliva — makes a noticeable difference. I often ask women to put their fork down between each mouthful, not out of strict discipline, but to invite presence and digestion.
Another key point I’ve seen over and over again is meal size. Large meals stretch the stomach and press against the diaphragm, which increases the chance of acid creeping upward. Breaking up food into smaller, more frequent meals — spaced throughout the day — tends to relieve pressure and allow digestion to stay gentle and steady.
Drinking water during meals can also be tricky. Too much fluid while eating can dilute stomach acid and lead to poor breakdown of food, which ironically increases reflux symptoms later. I usually suggest hydrating between meals, allowing the digestive process to stay balanced without being overwhelmed.
What to Avoid When Managing Pregnancy Reflux
Sometimes, finding relief isn’t just about what you add — but what you gently remove. I’ve seen women improve their symptoms almost overnight simply by becoming more aware of the subtle triggers in their daily routine.
Certain foods, for instance, have a tendency to relax the lower esophageal valve even further. This includes deeply fried dishes, overly spicy curries, and heavily processed snacks, which often sit in the stomach longer than gentler meals. Even seemingly innocent options like chocolate or mint teas can make reflux worse by softening that valve and allowing acid to creep upward.
Beyond food, there are habits that work against the body’s rhythm. Tight clothing around the waist can add pressure to the abdominal area, worsening symptoms, especially when sitting or bending. I also encourage women to reflect on their timing — lying down right after meals might feel tempting during pregnancy, but that single habit often leads to increased nighttime burning or regurgitation.
One of the most powerful changes is becoming more intuitive — listening to what foods, postures, and rhythms feel good, and which ones subtly make things worse. It’s not about strict restriction, but about gently creating a digestive environment where comfort is more likely.
Morning Habits That Set the Tone for Better Digestion
One thing I always share with my clients is how much the morning shapes the rest of the digestive day. After a night of rest, the body wakes up in a sensitive state. What you do — and how calmly you begin — can determine whether reflux remains quiet or flares up early.
A warm glass of lemon water, for example, can stimulate gentle gastric flow and awaken the intestines, especially when sipped slowly. Some women prefer a spoonful of aloe vera juice first thing — just enough to coat the stomach without overwhelming it. Either way, it’s less about the exact substance and more about the intention: start soft, warm, and mindful.
Eating breakfast without distraction, and chewing thoroughly, can train the body to expect digestion in a peaceful state. I often suggest sitting near a window or in a quiet space, and resisting the temptation to check phones or rush through emails while eating. When we bring ritual to breakfast, digestion responds with calm efficiency.
Stretching gently, moving the body before sitting too long, or even walking for ten minutes after breakfast can promote smoother transit and reduce pressure that might otherwise provoke reflux later in the day.
When Natural Approaches May No Longer Be Enough
While natural remedies work beautifully for many women — especially in the earlier stages — there are moments when symptoms become too severe to manage through lifestyle alone. I’ve seen women try everything right: mindful eating, elevated sleeping, ginger infusions, small meals — and still find themselves waking in the night with chest discomfort or struggling to eat enough because of the burn.
In these cases, I always emphasize that seeking medical support is not a failure. There are medications that are considered safe during pregnancy, and sometimes a short course can help restore balance so that natural measures become effective again. For example, antacids with calcium or magnesium are often recommended short-term and don’t carry the risks associated with stronger acid-blocking drugs.
What matters is getting enough nourishment and sleep — both essential for a healthy pregnancy. If natural tools stop working, the most important thing is to speak with your provider. I always tell women: you deserve comfort, and your baby deserves a mother who feels strong and well-fed.
The Emotional Power of Support: Partners, Family, and Rest
Reflux isn’t just a physical issue. I’ve seen how it can chip away at a woman’s emotional resilience — especially when it disrupts sleep night after night. This is where support becomes more than a luxury. It becomes a remedy in itself.
When a partner understands the condition — and doesn’t brush it off as “just heartburn” — it changes everything. I remember one client whose spouse started preparing smaller evening meals and made sure she had an extra pillow ready by bedtime. That simple presence gave her a sense of safety that no tea or tonic could replicate.
Family can help too — by giving you space to nap during the day, by supporting a gentler pace in the household, or simply by encouraging you to listen to your needs without guilt. Reflux tends to flare when stress rises. The more permission you have to rest, speak up, and slow down, the more likely your body is to heal.
Comfort is not just a matter of food or posture. Sometimes, it’s the result of being cared for — and allowing others to care for you.
Every Body Reacts Differently — and That’s Okay
One of the first things I remind every pregnant woman dealing with reflux is this: no two bodies respond the same way. I’ve worked with women who could drink citrus juice without issue, and others who felt burning from a single sip of peppermint tea. That doesn’t mean someone is wrong or failing — it simply means your body has its own unique rhythm.
During pregnancy, your digestion is shaped by hormonal shifts, physical changes in your organs, and even emotional energy. Some days, what felt fine yesterday might cause discomfort today. I always encourage women to tune into their experience without judgment. Sometimes, it’s helpful to keep a gentle journal, noting what foods, postures, or emotional states correlate with comfort — or discomfort.
You don’t need to follow every online list or article. What matters is how your specific body responds. That’s where the real wisdom lives — not in strict rules, but in quiet attention to your lived experience.
Natural Supplements That May Offer Relief
I’ve seen certain natural supplements offer real, gentle support — especially when used mindfully and under a provider’s guidance. One of the most effective options I’ve recommended is deglycyrrhizinated licorice, known as DGL. When taken before meals, it can coat and protect the esophagus and stomach lining, helping to reduce irritation without suppressing natural stomach acid.
Another option I’ve seen work well is slippery elm bark. It forms a soothing gel when mixed with water and taken before meals or at bedtime. For many women, especially those with sensitive digestion, this plant-based remedy provides a gentle barrier that keeps acid from aggravating the upper tract.
Chamomile and marshmallow root tea, when consumed slowly and in moderation, can also calm the digestive tract. I always recommend checking with a midwife or OB-GYN before starting anything new — especially during the delicate balance of pregnancy — but these options have earned my trust after seeing how often they’ve helped without side effects.
Evening Rituals for Better Sleep Without Heartburn
As the day winds down, the body needs help transitioning to rest — especially when reflux threatens to interrupt sleep. I always encourage women to treat the evening hours as sacred time. It’s not just about digestion; it’s about preparing the whole body to surrender and heal.
Finishing the last meal at least two hours before lying down can make a world of difference. I often suggest a short, gentle walk after dinner — even a few circles around the room — to keep things moving downward. A warm compress on the belly, or a cup of calming tea sipped slowly, can ease tension and invite the stomach to relax.
Lighting dim, soft lighting at night and lowering noise also sends a signal to the nervous system: it’s time to shift into parasympathetic mode, where digestion improves and heartburn decreases. I’ve seen how just ten minutes of mindfulness, breathwork, or journaling can set a woman up for a more restful night — not just physically, but emotionally too.
What to Expect After Giving Birth
One question I get often is: does reflux disappear after the baby arrives? The short answer is yes — for many women, the symptoms lessen significantly once the uterus shrinks and hormonal levels begin to stabilize. But it doesn’t happen overnight, and sometimes digestion needs time to reset fully.
I’ve worked with mothers who noticed improvement within days of delivery, especially if their reflux was tied to physical pressure from the growing belly. Others found that reflux lingered for several weeks, especially if stress, lack of sleep, or poor eating habits persisted.
Breastfeeding can also affect hormone levels and digestion, so I always encourage new mothers to continue the gentle habits they adopted during pregnancy. Warm foods, small portions, body positioning — these are all still relevant postpartum, even as the cause of reflux begins to resolve naturally.
Reflux during pregnancy is not forever. With time, support, and mindful habits, most women see their symptoms gradually fade as their bodies transition into a new phase.
FAQ – Natural Relief for Acid Reflux During Pregnancy
Can acid reflux really start in the first trimester?
Yes, and I’ve seen it many times. Even before the uterus begins to press on the stomach, hormonal changes — especially the rise in progesterone — can slow digestion and relax the valve between the stomach and esophagus. Some women begin feeling symptoms within the first few weeks.
What natural remedy has worked best for your clients?
In my experience, the combination of small, frequent meals, elevated sleeping, and a calming herbal tea like chamomile has brought consistent relief. But the single most effective tip I’ve seen is avoiding lying flat after eating — it changes everything for some women.
Is it safe to use baking soda for reflux during pregnancy?
I’ve had clients ask this a lot. While baking soda neutralizes acid quickly, I generally avoid recommending it during pregnancy unless approved by a doctor. It can lead to bloating, increase sodium intake, and disrupt natural pH balance — not ideal in such a sensitive state.
Does acid reflux during pregnancy affect the baby?
From what I’ve observed and discussed with medical professionals, reflux itself doesn’t harm the baby. But if it leads to poor appetite or malnutrition, it can indirectly affect fetal development. That’s why it’s so important to find relief and maintain healthy eating.
Can drinking milk help or hurt?
Some women swear by warm milk, others find it worsens the burn. I’ve seen both outcomes. In my experience, milk may soothe temporarily, but its fat and protein can later stimulate acid. If it helps, that’s great — but if not, there are gentler alternatives like oat or almond milk.
Why does reflux get worse at night?
Lying flat removes gravity’s help in keeping acid down. That’s why I always advise elevating the upper body and avoiding eating too close to bedtime. It’s one of the simplest and most effective changes a pregnant woman can make.
What’s the safest sleeping position for reflux?
From what I’ve seen in practice, sleeping on the left side is gentlest on digestion. It positions the stomach below the esophagus and reduces pressure. I’ve had women switch sides and notice improvement within days.
Are papaya enzymes or apple cider vinegar useful?
I’ve seen mixed results. Some women feel better with a small amount of apple cider vinegar before meals, others find it too harsh. Papaya enzymes are generally milder and may support digestion — but again, always check with your care provider first.
How often should I eat to avoid reflux?
I’ve found that eating smaller portions every two to three hours works best. Large meals stretch the stomach and increase acid pressure. Gentle, steady intake supports digestion and keeps acid levels more balanced.
What drinks are best for soothing reflux?
Based on what I’ve tried and seen, warm water with a slice of ginger or a mild herbal tea like marshmallow root works well. Avoid carbonated beverages, citrus juices, or anything with caffeine — those tend to make things worse.
Can stress really make reflux worse?
Absolutely. I’ve seen stress trigger or amplify symptoms even when the diet is clean. Stress alters breathing, tightens muscles, and slows down digestion. Emotional support and relaxation rituals can sometimes help more than any food change.
Do prenatal vitamins contribute to reflux?
Yes, sometimes. Iron in particular can irritate the stomach lining. I’ve had clients switch to low-iron formulations or take their vitamins with food — and the reflux improved. It’s worth discussing alternative brands with your OB if symptoms worsen after taking them.
Is heartburn during pregnancy linked to the baby’s hair growth?
It’s a fun myth — and surprisingly, I’ve heard it might have some truth. Some studies have linked high estrogen (which causes reflux) with fetal hair growth. But I tell my clients not to count on heartburn as a predictor. It’s more about physiology than baby fuzz.
When should I seek medical help for reflux?
If natural remedies no longer work, or if you’re losing sleep, appetite, or weight, it’s time to talk to your provider. I’ve seen reflux spiral into more serious discomfort, and timely medical support makes all the difference. There are safe options — you don’t have to suffer.
Will reflux go away after giving birth?
For most women I’ve worked with, yes. As hormone levels normalize and the uterus shrinks, the pressure eases and reflux often fades. That said, it’s still important to maintain gentle eating and sleep habits during the postpartum phase, especially while breastfeeding.










