Transverse Colon Cancer: Symptoms, Treatment, and Outlook
- What Is Transverse Colon Cancer?
- Symptoms of Transverse Colon Cancer
- Diagnostic Process and Imaging Techniques
- Staging and Spread Patterns of Transverse Colon Cancer
- Risk Factors Specific to Transverse Colon Cancer
- Surgical Treatment Approaches and Techniques
- Chemotherapy and Targeted Therapy in Management
- Transverse Colon Cancer Survival Rates by Stage
- Recurrence Risks and Monitoring After Treatment
- Liver Metastasis in Transverse Colon Cancer
- Molecular Subtypes and Personalized Treatment
- Understanding the Difference Between Transverse and Other Colon Cancers
- Psychosocial Impact and Support Systems
- Prevention Strategies and Early Detection
- Survival Rates and Prognosis Based on Stage
- Long-Term Follow-Up and Quality of Life
- FAQ
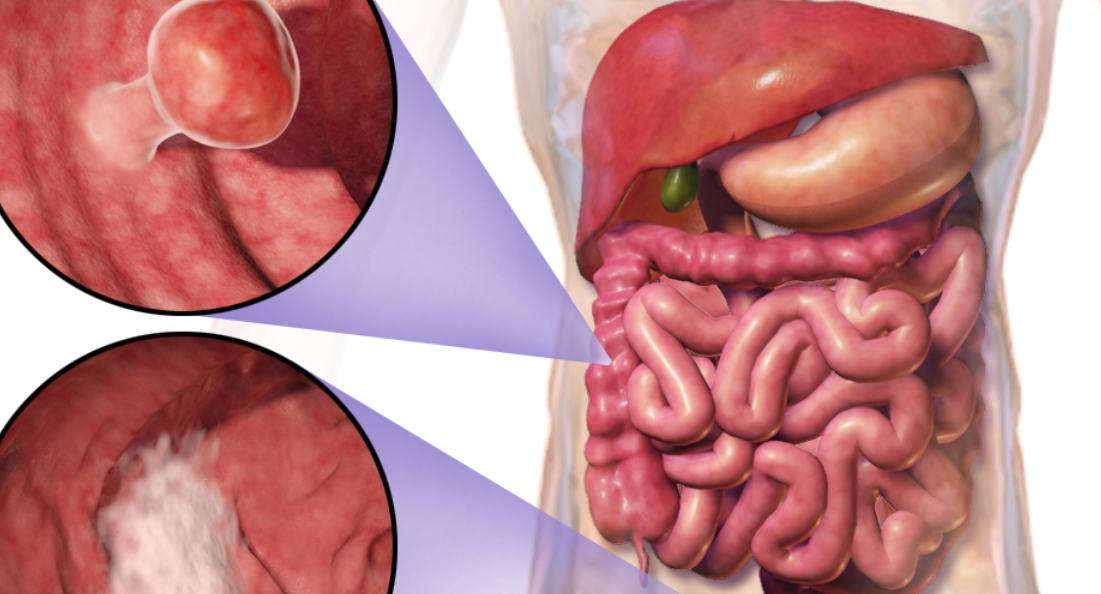
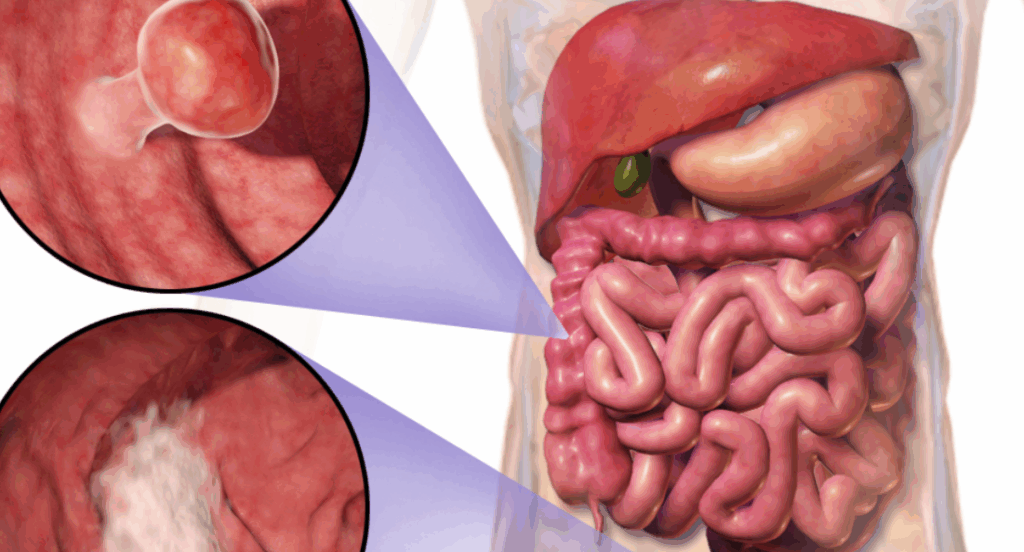
What Is Transverse Colon Cancer?
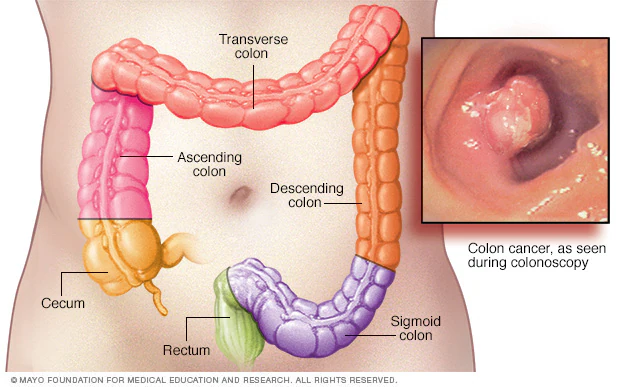
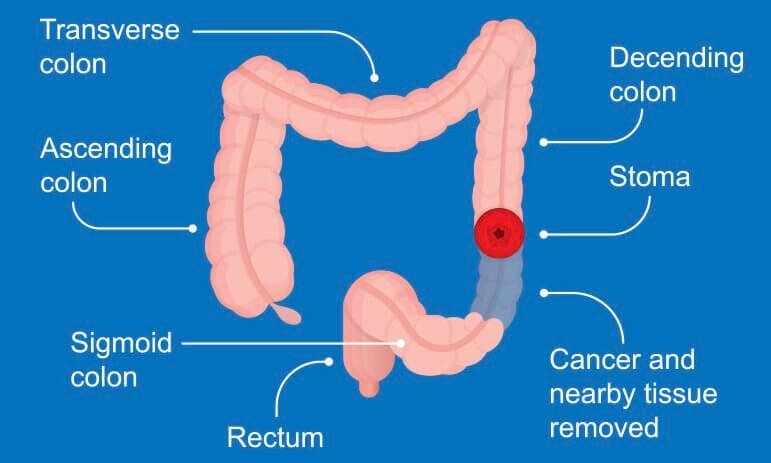
Transverse colon cancer refers to malignant growths that develop in the middle segment of the large intestine, specifically the portion that crosses the abdomen horizontally. It is classified as a subtype of colorectal cancer, though it represents a smaller percentage of total cases. The transverse colon sits between the ascending colon on the right and the descending colon on the left, which means any cancerous lesion here can potentially spread in both directions through the colon as well as nearby lymphatic structures.
Because of its central location, tumors in the transverse colon often go unnoticed longer than those in the rectum or sigmoid colon. The symptoms can be vague and non-localized, delaying diagnosis until the cancer is more advanced. Despite this, the biological behavior of transverse colon tumors doesn’t differ much from other colon cancers — they are usually adenocarcinomas and follow typical progression through the mucosal, submucosal, and muscular layers.
What sets transverse colon cancer apart is its surgical complexity and the variability of blood supply and lymphatic drainage in this area. Surgeons need to consider these anatomic nuances when planning resections and lymph node dissection.
Symptoms of Transverse Colon Cancer
The symptoms of transverse colon cancer are often nonspecific and can overlap with benign gastrointestinal issues, which is one of the reasons diagnosis is frequently delayed. Patients may report intermittent abdominal discomfort, changes in stool consistency, or unexplained fatigue. One of the distinguishing symptoms — though not exclusive — is cramping pain that shifts location across the upper abdomen.
Another key symptom can be partial obstruction, which may manifest as bloating, reduced appetite, and nausea. In contrast to rectal cancers, visible blood in stool is less frequent in transverse colon malignancies, though occult bleeding can still lead to iron-deficiency anemia over time.
In later stages, more dramatic symptoms such as weight loss, palpable masses, and persistent nausea may appear. Because of the overlap with irritable bowel syndrome and other functional disorders, early signs are often misattributed, delaying essential imaging and biopsies.
Diagnostic Process and Imaging Techniques
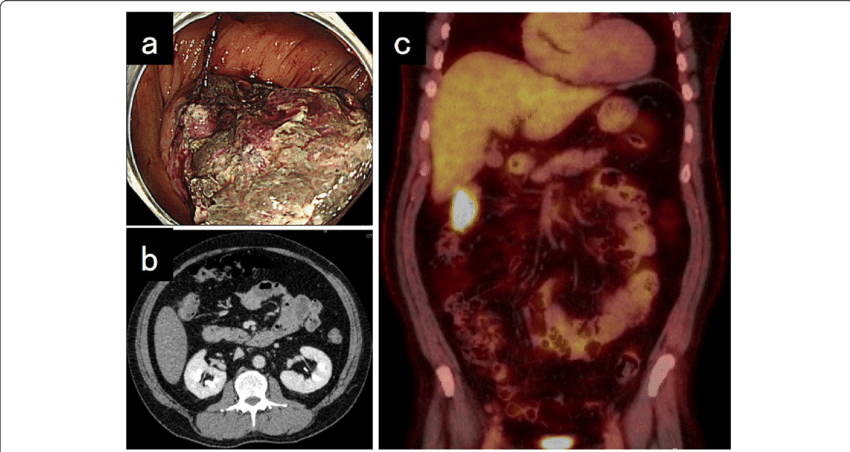
Diagnosing transverse colon cancer typically involves a combination of endoscopic, radiologic, and histopathologic methods. The first line of investigation is usually a colonoscopy, where a flexible scope is used to visually inspect the colon and obtain biopsy samples. However, the location of the transverse colon — suspended by the transverse mesocolon — sometimes makes full visualization technically difficult, especially if the bowel is poorly prepped.
In these cases, contrast-enhanced CT scans or virtual colonoscopy (CT colonography) can help visualize obstructive masses or wall thickening. MRI may also be used, particularly when evaluating lymph node involvement or liver metastasis. Blood tests, such as carcinoembryonic antigen (CEA), can serve as tumor markers, though they lack specificity and are better suited for post-treatment surveillance.
Histopathological confirmation remains the gold standard. Once biopsy samples are obtained, they are examined for glandular architecture, degree of dysplasia, and evidence of invasive growth. Immunohistochemistry may also be applied to determine the molecular subtype, which helps guide chemotherapy or targeted therapy.
Staging and Spread Patterns of Transverse Colon Cancer
Once diagnosed, transverse colon cancer is staged according to the TNM system, which assesses the tumor’s depth of invasion (T), lymph node involvement (N), and presence of distant metastasis (M). Stage I represents confined tumors within the mucosa or submucosa, while Stage IV indicates distant spread, often to the liver, lungs, or peritoneum.
Due to its mid-abdominal position, transverse colon tumors can potentially spread in both rightward and leftward directions along the colon, complicating surgical planning. Lymphatic spread often follows the middle colic artery, requiring dissection of both right and left mesocolic nodes. In some cases, this necessitates an extended hemicolectomy rather than a localized segmental resection.
Liver metastasis is a common site of spread, particularly when cancer invades the portal venous system. Peritoneal involvement can also occur if the tumor perforates the serosa. These advanced cases often require multimodal treatment, including chemotherapy, cytoreductive surgery, and hyperthermic intraperitoneal chemotherapy (HIPEC). For more information on stages and metastasis, see Does tattoo removal cause cancer, which explains the interaction between laser technology and the lymphatic system
Risk Factors Specific to Transverse Colon Cancer
While many risk factors for colorectal cancers are shared across different anatomical regions, transverse colon cancer has its own nuances due to its anatomical location and delayed symptom presentation. Age remains a predominant factor, with most cases diagnosed after age 50, though early-onset cases are increasingly recognized, especially in genetically predisposed individuals.
Dietary habits, such as high consumption of red and processed meats combined with low fiber intake, increase the risk of adenomatous polyp formation, some of which may localize in the transverse segment. Chronic inflammatory bowel diseases, particularly ulcerative colitis, can involve the transverse colon and increase cancer risk through continuous mucosal inflammation and dysplasia.
Genetic syndromes like Lynch syndrome and familial adenomatous polyposis (FAP) also predispose patients to malignancies in this region. Importantly, individuals with prior abdominal radiation or a history of polyps in the transverse colon require closer surveillance. Sedentary lifestyle, obesity, smoking, and alcohol abuse add further layers of risk, making prevention strategies multifactorial.
Surgical Treatment Approaches and Techniques
Surgical removal remains the cornerstone of curative treatment for localized transverse colon cancer. The complexity of its location often necessitates a more nuanced approach than standard right or left hemicolectomy. Most commonly, an extended right hemicolectomy or transverse colectomy is performed, depending on tumor proximity to the hepatic or splenic flexures.
The procedure involves mobilizing the transverse colon from its mesentery, ligating the middle colic artery, and ensuring adequate lymphadenectomy. Surgeons must account for variations in vascular anatomy, as accessory or replaced colic arteries may alter the resection plan. Achieving negative margins is critical, especially in tumors with subserosal spread or lymphovascular invasion.
Laparoscopic colectomy is increasingly favored due to faster recovery and reduced postoperative complications. However, for bulky tumors or those with adjacent organ invasion, open surgery may be preferred. Postoperative recovery depends on early mobilization, bowel function restoration, and infection prevention. Complications like anastomotic leakage, ileus, or wound dehiscence, though uncommon, require close monitoring. Surgical intervention is especially critical in the presence of concomitant tumors – for more details, see What is PTP1B in breast cancer, which describes the effect of proteins on the regulation of tumor growth
Chemotherapy and Targeted Therapy in Management
Systemic therapy plays a crucial role in both adjuvant and palliative settings for transverse colon cancer. Adjuvant chemotherapy is typically offered for Stage III and some high-risk Stage II patients after surgical resection, especially when features such as lymphovascular invasion or poor differentiation are present.
Standard regimens include fluoropyrimidines (such as 5-FU or capecitabine) combined with oxaliplatin, known as FOLFOX or CAPOX. These regimens aim to eradicate microscopic residual disease and reduce recurrence risk. In metastatic cases, therapy becomes more complex and is tailored based on molecular profiling of the tumor.
Mutations in KRAS, NRAS, and BRAF genes influence the use of targeted agents such as anti-EGFR monoclonal antibodies (e.g., cetuximab) or VEGF inhibitors (e.g., bevacizumab). Microsatellite instability-high (MSI-H) tumors may respond well to immune checkpoint inhibitors like pembrolizumab. These approaches have reshaped the outlook for many patients, though side effects remain significant and require expert management.
Transverse Colon Cancer Survival Rates by Stage
| Stage | Description | 5-Year Survival Rate | Key Factors Influencing Outcome |
| Stage I | Confined to inner layers | ~90% | Complete resection, no lymph nodes involved |
| Stage II | Tumor penetrates muscular layer | ~75% | Lymphovascular invasion, poor differentiation |
| Stage III | Lymph node involvement | ~55–65% | Number of nodes affected, molecular subtype |
| Stage IV | Distant metastasis (e.g., liver) | ~10–15% | Response to systemic therapy, resectability of metastases |
Survival rates depend not only on stage but also on surgical margins, response to chemotherapy, and patient comorbidities. Regular follow-up and imaging play a critical role in improving long-term outcomes.
Recurrence Risks and Monitoring After Treatment
Recurrence is a persistent concern for individuals treated for transverse colon cancer, particularly within the first three years post-resection. While recurrence rates are closely tied to the initial stage at diagnosis, other factors like lymph node involvement, tumor margins, and molecular characteristics significantly influence outcomes.
Patients typically undergo routine follow-ups every 3–6 months for the first two years and then every 6–12 months thereafter. Monitoring involves physical exams, carcinoembryonic antigen (CEA) blood tests, colonoscopy, and cross-sectional imaging such as CT or MRI. CEA trends, although not specific, can be useful indicators of recurrence, particularly in Stage III or IV patients.
Tumor recurrence can manifest locally at the anastomosis site or metastatically, most often in the liver or lungs. Surveillance protocols also evaluate emerging treatment-related complications. Patient adherence to the monitoring schedule is critical, as early detection of recurrence improves options for curative re-intervention or prolonged survival through systemic therapy.
Liver Metastasis in Transverse Colon Cancer
The liver is the most common site of distant spread in transverse colon cancer due to portal circulation. In many cases, liver metastases are diagnosed simultaneously with the primary tumor (synchronous) or within the first 2–3 years post-treatment (metachronous). The management of liver metastasis is highly individualized and multidisciplinary.
Surgical resection remains the gold standard for patients with resectable liver-only disease. Hepatectomy offers the best chance for prolonged survival and even cure in select cases. In patients with multiple, bilateral, or deep-seated metastases, ablative techniques such as radiofrequency ablation (RFA) or stereotactic body radiation therapy (SBRT) may be considered.
Systemic chemotherapy, with or without biologic agents, is frequently used to downsize unresectable disease (conversion therapy). Response assessment via imaging guides the decision to operate or continue palliative care. Survival for patients with resectable liver metastases can exceed five years, underscoring the importance of careful selection and timing of interventions. Like liver metastases, the metastatic behavior of some tumors is discussed in stage 4 neuroendocrine cancer spread to liver life expectancy
Molecular Subtypes and Personalized Treatment
Advancements in genomic analysis have revealed that transverse colon cancer exhibits diverse molecular characteristics, which influence treatment response and prognosis. MSI-H (microsatellite instability-high) tumors, often associated with Lynch syndrome, tend to be less responsive to standard chemotherapy but highly susceptible to immunotherapy.
Conversely, MSS (microsatellite stable) tumors are more likely to harbor mutations in KRAS, NRAS, or BRAF genes. KRAS or NRAS mutations preclude the use of EGFR inhibitors like cetuximab or panitumumab, while BRAF mutations are associated with poorer prognosis but may respond to combination regimens including BRAF inhibitors.
Tumor mutational burden (TMB), CpG island methylator phenotype (CIMP), and chromosomal instability are additional stratifiers used in research and, increasingly, clinical care. These markers are reshaping colon cancer management, helping oncologists select therapies with higher efficacy and lower toxicity. A similar approach to biomarkers is used in other pathologies – see do parasites cause breast cancer, where the influence of microorganisms and their proteins on cancer is also studied.
Understanding the Difference Between Transverse and Other Colon Cancers
Transverse colon cancer is anatomically and behaviorally distinct from cancers arising in other segments of the colon. The transverse colon stretches horizontally across the abdomen and is suspended by the transverse mesocolon, making surgical access and lymphatic drainage different from ascending or descending colon cancers.
The embryological origin of the transverse colon also straddles midgut and hindgut territories, resulting in mixed vascular and lymphatic supplies. This anatomical duality impacts the choice of surgical technique and extent of resection needed for clear margins. Symptomatically, tumors here are often more subtle and present later than right-sided cancers (which may cause anemia) or left-sided cancers (which may cause obstruction).
These distinctions are critical for radiologists interpreting imaging, surgeons planning resections, and oncologists choosing systemic therapies. Recognizing these nuances improves staging accuracy, surgical outcomes, and survival projections.
Psychosocial Impact and Support Systems
A diagnosis of transverse colon cancer often brings significant psychological stress. Patients may experience anxiety, depression, fear of recurrence, or body image concerns post-surgery—especially when a temporary or permanent ostomy is involved. These challenges affect not only the patient’s mental health but also treatment compliance and overall recovery.
Effective support systems—including counseling, social workers, cancer support groups, and patient navigators—play a vital role in emotional recovery. Cognitive behavioral therapy (CBT), mindfulness-based stress reduction, and peer-led survivorship programs have shown evidence-based benefits in reducing distress. Family education and engagement further strengthen the patient’s resilience by reducing isolation and fostering understanding.
Navigating these emotional landscapes is just as important as medical care. Oncology teams are increasingly integrating mental health screening and psychosocial interventions into routine cancer management pathways.
Prevention Strategies and Early Detection
While not all cases of transverse colon cancer are preventable, several modifiable risk factors can be targeted to reduce incidence. These include smoking cessation, limiting red and processed meat intake, increasing dietary fiber, and maintaining a healthy weight. Physical activity and reduced alcohol consumption also lower risk through improved metabolic and immune regulation.
Screening programs are among the most effective tools in colorectal cancer prevention. Colonoscopy remains the gold standard, allowing for the detection and removal of pre-cancerous polyps. Fecal immunochemical tests (FIT), stool DNA testing, and CT colonography serve as alternative or complementary methods depending on patient risk and access.
For high-risk groups—such as those with a family history of colorectal cancer or hereditary syndromes like Lynch syndrome—screening should begin earlier and occur more frequently. These proactive measures dramatically improve outcomes by enabling early-stage diagnosis and curative intervention. The topic of early detection and prevention is also relevant for other pathologies, see What is PTP1B in breast cancer?
Survival Rates and Prognosis Based on Stage
Prognosis in transverse colon cancer varies significantly by stage at diagnosis, molecular subtype, and response to treatment. Below is a comparative table outlining estimated 5-year survival rates across stages.
| Stage of Transverse Colon Cancer | Description | Estimated 5-Year Survival Rate |
| Stage I | Tumor limited to mucosa/submucosa | 90–95% |
| Stage II | Tumor invades muscularis, no nodes | 75–85% |
| Stage III | Regional lymph node involvement | 50–70% |
| Stage IV | Distant metastases (e.g., liver, lung) | 10–20% |
These figures are general estimates based on SEER data and may differ based on individual factors. Personalized prognosis requires integrating tumor biology, patient age and comorbidities, and access to advanced treatment modalities.
Importantly, emerging therapies and surgical advancements continue to shift survival expectations upward, especially in patients with Stage III and even Stage IV disease when treated aggressively and monitored closely.
Long-Term Follow-Up and Quality of Life
Survivorship care extends well beyond the conclusion of treatment. Long-term follow-up focuses on several critical domains: monitoring for recurrence, managing late effects of treatment, ensuring proper nutrition, and optimizing physical and emotional wellbeing.
Common late effects in transverse colon cancer survivors include bowel habit changes, adhesions, fatigue, neuropathy (especially from oxaliplatin), and osteopenia from steroid use. Nutritionists may assist in developing high-fiber, low-fat diets to normalize bowel function. Physical therapy and guided exercise are essential for restoring stamina and mitigating post-treatment fatigue.
Oncologists also coordinate with primary care providers to address cardiovascular health, diabetes risk, and bone density. Survivorship plans increasingly include digital tracking tools and survivorship clinics that offer structured care plans tailored to individual needs. Quality of life is measured not just by survival, but by how well patients return to meaningful, active lives.
FAQ
What is transverse colon cancer and how common is it?
Transverse colon cancer is a form of colorectal cancer that originates in the horizontal section of the colon, which crosses the abdomen. Although less common than cancers in the sigmoid or rectal areas, it represents a significant clinical concern due to its central location and varied symptom profile. Its detection often requires imaging or colonoscopy, as symptoms may mimic gastrointestinal disorders.
What are the early warning signs of transverse colon cancer?
Early signs can include abdominal bloating, unexplained fatigue, anemia, and changes in bowel habits, such as intermittent constipation and diarrhea. Because these symptoms are nonspecific, many patients mistake them for dietary issues or irritable bowel syndrome, delaying diagnosis. Blood in the stool may occur but is less frequent than in cancers of the distal colon.
How is transverse colon cancer diagnosed?
Diagnosis typically begins with a colonoscopy, which allows direct visualization and biopsy of suspicious lesions. CT scans and MRI are used for staging, while blood tests (including CEA tumor marker) support the diagnostic picture. Advanced diagnostics may involve PET-CT or genomic profiling in certain cases.
What treatment options are available for transverse colon cancer?
Treatment commonly involves surgical resection of the tumor-bearing section of the colon, followed by chemotherapy depending on stage and lymph node involvement. Radiation therapy is rarely used due to the location of the transverse colon but may be considered if cancer has spread to nearby structures.
Is chemotherapy necessary in all cases of transverse colon cancer?
Not always. For Stage I cancers, surgery alone may be curative. Chemotherapy is typically recommended for Stage III and selectively for high-risk Stage II cases. The decision is based on pathology findings, patient health status, and molecular characteristics of the tumor.
What is the role of immunotherapy in treating this cancer?
Immunotherapy may be considered in cases where the tumor shows microsatellite instability-high (MSI-H) or mismatch repair deficiency (dMMR). These biological markers predict better response to PD-1 inhibitors. This option is most often explored in metastatic or recurrent settings.
Can lifestyle changes reduce the risk of recurrence?
Yes. Maintaining a healthy body weight, adopting a high-fiber and low-red-meat diet, engaging in regular physical activity, and avoiding smoking and excess alcohol all contribute to lower recurrence risk. Routine follow-up care with periodic imaging and colonoscopy is also essential in catching recurrence early.
How does transverse colon cancer differ from other colorectal cancers?
Its central position in the colon means that symptoms are often delayed or non-specific, making early detection more difficult. Surgical management can also be more complex due to the proximity of blood vessels and surrounding organs. Additionally, right-sided colon cancers (like many transverse ones) often present differently than left-sided ones in terms of molecular profile and prognosis.
What is the prognosis for Stage IV transverse colon cancer?
Stage IV disease indicates distant metastasis, most commonly to the liver or lungs. Prognosis depends on factors such as performance status, number and location of metastases, and response to treatment. With modern chemotherapy and targeted agents, some patients achieve disease control for multiple years, though 5-year survival rates remain low.
Is it possible to live a normal life after surgery for transverse colon cancer?
Many patients return to their normal routines after recovery, though some experience long-term changes in bowel habits or diet. Adaptation typically occurs over time, and with proper medical and nutritional support, most individuals report a good quality of life. Emotional resilience and ongoing follow-up play an important role.
How often should I get screened if I have a family history?
Individuals with a first-degree relative diagnosed with colorectal cancer should begin screening 10 years before the age of the family member’s diagnosis or at age 40, whichever comes first. Genetic counseling may also be recommended, especially in families with multiple affected members.
What are the most common sites of metastasis for transverse colon cancer?
The liver is the most frequent site, followed by the lungs and peritoneum. Metastasis to distant lymph nodes or even the brain can occur but is less common. Understanding metastatic patterns helps guide imaging and treatment decisions in advanced stages.
Are there any long-term side effects from treatment?
Yes, common long-term effects include peripheral neuropathy from chemotherapy, fatigue, gastrointestinal dysfunction, and, in some cases, complications from surgery such as adhesions or hernias. These effects are manageable but require monitoring and supportive care to maintain quality of life.
Can transverse colon cancer come back after treatment?
Yes, recurrence can occur locally or as distant metastasis, most often within the first three years after treatment. This is why a structured follow-up plan including regular scans, blood tests, and colonoscopies is critical. Patients are also advised to report new symptoms promptly.
What should I ask my doctor if I’ve been diagnosed with this cancer?
You should ask about the stage of your cancer, treatment options and their side effects, surgical approach, prognosis, and whether genetic testing is recommended. Inquire about dietary guidance, emotional support services, and how your treatment plan will be monitored over time.