Sunspot or skin cancer (подробно – что это, как отличаются, может ли переродиться в рак, что делать и пр)
- 1. Introduction
- 2. Sunspots (Solar Lentigines)
- 3. Skin Cancer
- 4. Actinic Keratosis: The Precancerous Lesion
- 5. Differentiating Sunspots from Skin Cancer
- 6. Diagnosis and Monitoring
- 7. Treatment Modalities
- 8. Prevention Strategies
- 9. Psychological and Social Considerations
- 11. Frequently Asked Questions (FAQs)
- Closing Thoughts
Introduction
If you’ve ever stood in front of the mirror and wondered whether that new speck on your shoulder is just a harmless sunspot—or something more sinister—you’re not alone. The human skin is a living journal of our time spent under the sun, and sometimes, the ink it uses isn’t as innocent as we’d like. So how do you tell the difference between an ordinary sunspot and a warning sign of skin cancer? And is there ever a point where a simple sunspot becomes something to worry about?

Let’s be clear from the start: not every spot is dangerous. In fact, most aren’t. But some are, and the earlier you can distinguish between the two, the better your chances are of addressing it effectively and calmly—without panic, but also without delay.
Why This Topic Matters
Skin cancer is the most common form of cancer worldwide, and it’s also one of the most preventable. At the same time, benign sunspots—often called solar lentigines—are also incredibly common, especially among people over 40 or those who’ve spent a good deal of time in the sun. The problem arises when the lines blur, both figuratively and literally. A flat brown mark on your cheek might look like the sunspot you’ve had for years, but what if it starts changing shape? What if it’s new? What if it itches, bleeds, or darkens?
This article exists for exactly those moments of doubt. You’ll learn how sunspots form, what skin cancers actually look like (and how they behave), and where the overlap ends. Most importantly, we’ll dive into what you should do when you’re unsure, because relying on Google image searches and well-meaning Reddit threads is a recipe for anxiety—not clarity.
Common Early Questions
Let’s tackle a few of the questions that typically pop up early on when people start researching this topic:
- Can a sunspot turn into cancer?
Not exactly. A sunspot doesn’t “transform” into cancer the way a mole can sometimes evolve into melanoma. But—and this is critical—sunspots are signs that your skin has absorbed a fair amount of UV damage over the years. That sun damage is a known contributor to skin cancer risk. So while the spot itself might not be dangerous, it’s waving a little flag that says, “Hey, your skin’s been through a lot. Keep an eye on things.” - How can I tell the difference at home?
There are visual cues that dermatologists use, and we’ll go over those in detail. But no amount of online sleuthing replaces the certainty of a trained eye, especially if the spot in question has changed recently. Think of your skin as a living landscape—if something new crops up or an old hill suddenly grows a strange peak, it’s worth investigating. - Is this only a concern for fair-skinned people?
While people with lighter skin are more prone to both sunspots and skin cancer, no one is immune. Melanin does offer some natural protection, but it’s not a shield. People of all skin tones can develop skin cancers, and in darker-skinned individuals, those cancers are often diagnosed later, which can lead to worse outcomes.
The Stakes and the Strategy
This isn’t just about knowing what to worry about and what to ignore. It’s about reclaiming some agency over your health. Once you understand what’s happening with your skin, you’re less likely to oscillate between total denial and late-night doomscrolling. And even if you do find something suspicious, that knowledge—combined with swift action—can literally save your life.
In the sections that follow, we’ll unpack what sunspots actually are (hint: they’re not freckles, and they’re not age spots either), walk through the biology of different types of skin cancer, and offer side-by-side comparisons that make spotting the differences far more manageable. We’ll also get into lesser-known but crucial details, like actinic keratosis (a “pre-cancer” that sits on the borderline) and modern treatment options that are both effective and often minimally invasive.
By the time we’re done, you won’t just be more informed—you’ll be capable of acting wisely, either to calm your nerves or to take the right next step with confidence.
Sunspots (Solar Lentigines)
Let’s talk about sunspots. Not the solar flares millions of miles away, but the ones right there on your skin — the small, flat, brownish patches that seem to appear out of nowhere after a summer well spent or, let’s be honest, decades of intermittent sunscreen use. You might have noticed one on your cheek, the back of your hand, or your shoulders. Maybe it appeared after a beach vacation, or maybe it’s just always been there, blending in with freckles or age spots. Whatever the case, these sun-induced blotches tend to raise the same question at some point: Should I be worried?
The short answer: usually no. But “usually” is doing a lot of work in that sentence, and that’s where it’s worth digging deeper.
What Exactly Are Sunspots?
Medically, these are called solar lentigines — “lentigo” being the Latin word for lentil, which tells you something about their size and shape. They’re pigment-heavy patches that develop in response to ultraviolet (UV) radiation. When your skin is repeatedly exposed to the sun, it goes into protective mode. Your melanocytes (those pigment-producing cells) respond by overproducing melanin in certain areas, almost like building a little umbrella of pigment. The result? A flat, round or oval patch that’s darker than the surrounding skin.

Now, here’s what’s important: a sunspot is not a mole, and it’s not a freckle either. Freckles tend to appear and fade with sun exposure — they’re dynamic. Sunspots, by contrast, tend to hang around. They’re a sign of cumulative damage. Like smoke stains on the ceiling after years of lighting candles — they don’t just wipe off with time.
Why Do Some People Get Them While Others Don’t?
Genetics play a role, absolutely. People with fair skin (Fitzpatrick skin types I–III) are more prone to both sunspots and sun damage in general. But it’s not a fair-skinned-only club. Anyone who’s spent a significant amount of time in the sun without protection — especially over many years — can develop them. That includes outdoor athletes, lifeguards, gardeners, and yes, even people who swear they “don’t burn, just tan.”
Interestingly, sunspots tend to multiply with age — not because aging causes them directly, but because aging represents cumulative exposure. They’re less about “getting older” and more about “getting more sunlight over time.”
So… Are They Harmless?
In the overwhelming majority of cases, yes. Sunspots are benign, meaning they aren’t dangerous and don’t carry the threat of spreading or turning malignant. But — and this is where nuance matters — they’re markers of long-term UV exposure, which is itself a major risk factor for skin cancer. So while the spot itself isn’t a problem, the skin that produced it might have other changes going on beneath the surface. Think of them as red flags waving gently, not panic sirens screaming.
This brings us to a common fear: Can a sunspot turn into cancer?
It’s a reasonable question, especially if you’ve noticed a new spot that looks suspiciously darker than the rest or is changing shape. But the science is relatively clear: sunspots don’t transform into skin cancer. That’s not how skin cancer usually develops. Instead, cancer tends to arise independently — often in areas of sun-damaged skin, sometimes even right next to sunspots, but not from them directly. It’s a bit like seeing weeds growing in cracked pavement; the crack didn’t become the weed, but both are signs that the surface is stressed.
How Can You Tell If It’s Just a Sunspot?
This is where things get tricky for the untrained eye. A classic sunspot is:
- Flat and well-defined
- Tan to dark brown
- Uniform in color
- Found on sun-exposed areas like the face, hands, chest, and shoulders
- Persistent, but generally unchanged over time
If a spot meets those criteria and hasn’t changed in months or years, chances are good it’s just a sunspot. That said, dermatologists don’t play guessing games — they use tools like dermatoscopes to inspect the structure of pigment beneath the skin’s surface. And when there’s any doubt, a simple biopsy offers definitive answers.

And remember: sunspots may not be medically worrisome, but that doesn’t mean everyone wants to keep them. Some people find them cosmetically bothersome, and fortunately, there are treatments. These range from prescription-strength topical lightening agents to laser therapies and chemical peels. The results vary depending on skin tone, spot depth, and the chosen method — but it is possible to fade or even eliminate them.
When to Be Suspicious
So, when should a spot that looks like a sunspot raise your concern? Dermatologists often flag the following:
- Changes in size, color, or shape
- New symptoms, such as itching, bleeding, or crusting
- A spot that looks different from all your others — the so-called “ugly duckling” sign
Even a benign spot can be suspicious if it doesn’t behave like the rest. And here’s where we’ll bridge into the next section: not every sun-related spot is as innocent as it seems. Some are warning shots. Others are actual malignancies masquerading as freckles or age spots.
Before you start second-guessing every mark on your arms, though, let’s shift gears. In the next part, we’ll break down the different types of skin cancer — what they look like, how they form, and why catching them early is absolutely crucial.
Skin Cancer
Now that we’ve explored sunspots—the quiet aftermath of sun exposure—it’s time to talk about the darker side of UV damage: skin cancer. This is the part of the conversation where things get serious, but don’t worry—we’re not going to launch into alarmism or bury you in medical jargon. Instead, we’re going to get practical, informed, and honest. Because understanding skin cancer is the key to catching it early, treating it effectively, and, ideally, preventing it altogether.
So What Is Skin Cancer, Exactly?
At its core, skin cancer is what happens when certain cells in your skin start growing out of control. And unlike sunspots, which are just a cosmetic signal of sun exposure, skin cancer is an actual mutation—a breakdown in the cellular instruction manual. It’s the difference between a wall getting a stain and that wall developing a structural crack. One’s a nuisance; the other compromises the integrity of the whole system.
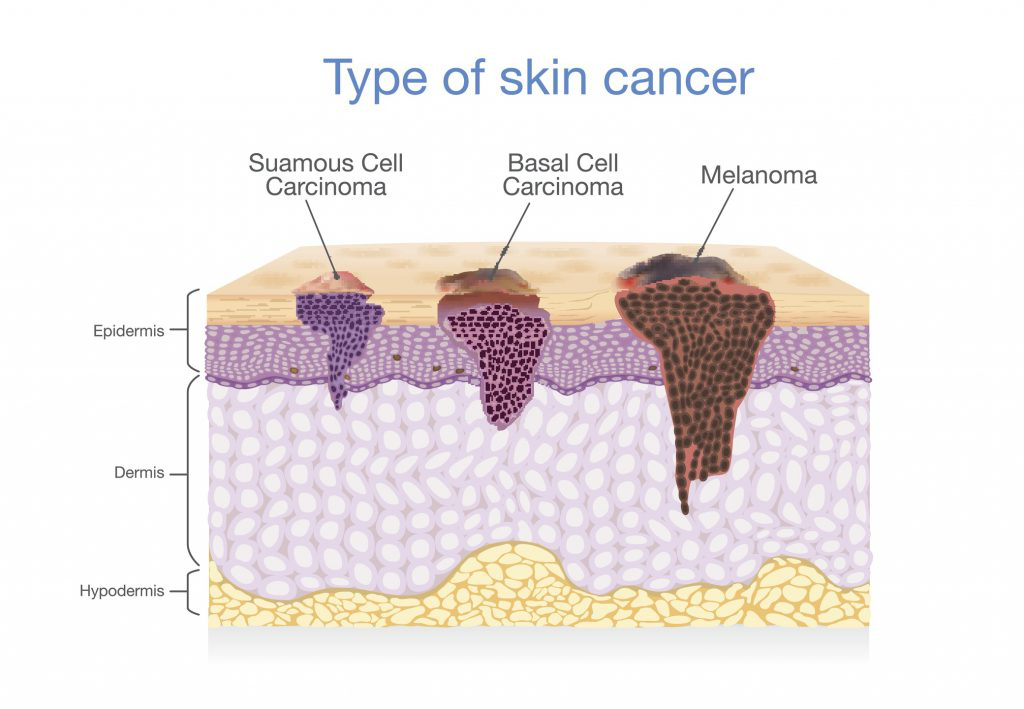
But here’s the thing: skin cancer isn’t one single disease. It’s an umbrella term that includes multiple distinct conditions, each with its own risk level, behavior, and appearance. The three major players are:
- Basal cell carcinoma (BCC)
- Squamous cell carcinoma (SCC)
- Melanoma
Let’s unpack each of these with clarity, nuance, and a healthy respect for the science.
Basal Cell Carcinoma (BCC): The Most Common Culprit
Basal cell carcinoma is by far the most common type of skin cancer—not just in the skin cancer category, but across allcancers. Millions of new cases are diagnosed each year, and the overwhelming majority of them are caught early and treated successfully.
So what does BCC look like? That’s the frustrating part—it varies. It might show up as a pearly bump, a waxy patch, a small sore that won’t heal, or a reddish area that bleeds a little and then seems to scab over… only to come right back. The pattern here is stubbornness. These lesions linger. They don’t go away, and they seem to resist the normal healing process.
BCC grows slowly and rarely spreads to other parts of the body. But that doesn’t mean it’s harmless. Left untreated, it can burrow deeper, damaging underlying tissues, cartilage, even bone. It can disfigure. So no, it’s not “just a skin cancer.” It needs to be taken seriously, even when it looks deceptively minor.
Squamous Cell Carcinoma (SCC): The Middle Ground
Squamous cell carcinoma is a bit more aggressive than BCC and slightly more likely to spread (especially if it goes ignored for too long), but still highly treatable when caught early. SCC arises from squamous cells, which are found in the outer layers of your skin.
It often appears as a rough, scaly patch or a firm, red nodule. Sometimes it crusts or bleeds. Sometimes it resembles a wart. Again, the variety makes it tricky, but the unifying theme is that it doesn’t behave like normal skin. It’s persistent, maybe a little angry-looking. And it often pops up in areas that get lots of sun: the scalp, the backs of the hands, the tops of the ears.
Is SCC deadly? In most cases, no—but it can metastasize if given enough time and space, especially in people with weakened immune systems or other underlying health conditions. That’s why catching it early isn’t just a good idea—it’s a medical priority.
Melanoma: The Dangerous One
And then we come to melanoma, the wild card. Melanoma is much less common than BCC or SCC, but it’s far more dangerous. Why? Because it’s the type of skin cancer most likely to spread—first to lymph nodes, then to organs. And once it spreads, treatment becomes much more complex.
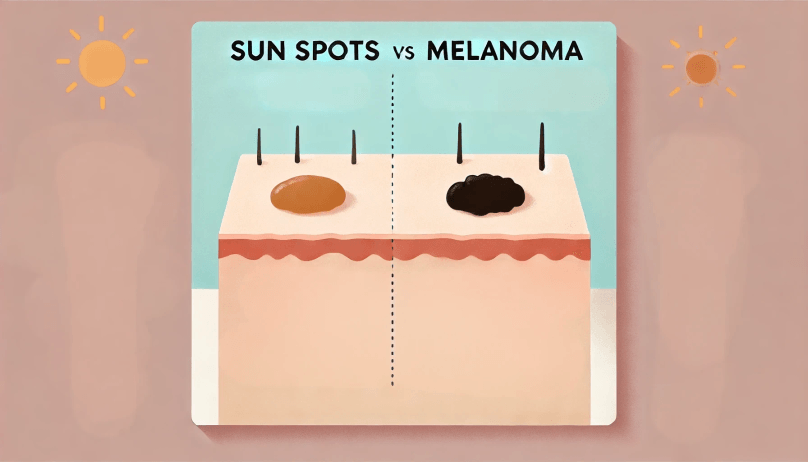
Melanoma begins in the melanocytes—the very same cells responsible for sunspots and pigmentation. This is partly why it can look like a mole. But not all moles are melanomas, and not all melanomas arise from existing moles. Some come out of seemingly clear skin.
This is why dermatologists teach the ABCDE rule, which we’ll dive into in more detail later. In short, you’re looking for moles or spots that are:
- Asymmetric
- Have irregular borders
- Display multiple colors
- Are diameter > 6mm
- Or are evolving in appearance
People often ask, “How fast does melanoma grow?” The answer: it depends. Some melanomas (nodular melanoma, for example) grow alarmingly fast—over weeks, not years. Others develop more gradually. But the real takeaway is this: if something on your skin is changing quickly or looks fundamentally different from everything else, don’t wait. Get it checked.
But Isn’t Skin Cancer Obvious?
This is the dangerous myth. People expect skin cancer to be grotesque, unmistakable, and clearly “bad.” But in reality? Skin cancer often looks boring. It masquerades as a pimple, a sunspot, a flaky patch. It hides in plain sight. And because the skin regenerates constantly, we’re used to seeing little things appear and disappear.
So what’s the best way to deal with that ambiguity? Awareness. Attention. Regular self-checks and professional skin exams. Not panic, but vigilance.
We’ll explore how to do that—how to monitor your own skin intelligently—in a later section. But for now, just remember: your skin is the most visible organ you have. And it’s talking to you all the time. You just need to learn its language.
Actinic Keratosis: The Precancerous Lesion
Now that we’ve laid the groundwork with sunspots and skin cancer, it’s time to zoom in on something that lives in the gray zone: actinic keratosis, also known as solar keratosis. If you’ve never heard of it before, you’re not alone—this condition doesn’t get nearly the attention it deserves. Yet it’s incredibly common, medically significant, and, quite frankly, under-discussed for how often it shows up in clinical practice.
So what is actinic keratosis, and why does it matter? In a nutshell, it’s your skin’s version of a warning shot. A gentle but firm tap on the shoulder saying, “Hey, something’s not right here. Not yet cancer… but not entirely safe either.”
What It Is (And What It’s Not)
Actinic keratosis (AK for short) is a precancerous lesion caused by cumulative sun damage. These are areas where UV exposure has altered the DNA of skin cells—specifically keratinocytes—but hasn’t quite pushed them over the edge into full-blown squamous cell carcinoma. Think of it as cellular dysplasia: the architecture is off, but it hasn’t lost all control. Yet.
The name “actinic” refers to ultraviolet radiation, and “keratosis” means thickening of the skin. Put those together and you get a pretty apt description: thickened, UV-damaged skin. But that doesn’t mean these lesions are large or dramatic. In fact, they can be frustratingly subtle.
Often, patients don’t even notice them visually—they feel them first. The classic AK is a rough, sandpaper-like patch on sun-exposed skin: scalp, face, ears, neck, forearms. It might feel dry or crusty, and it may flake or even bleed slightly with irritation. Some are pink. Others are tan. A few are completely skin-colored.
And here’s the kicker: most people over 50 have at least one, whether they know it or not.
Why You Should Pay Attention
This is where things get serious. While AKs themselves are benign, they aren’t static. About 10% of actinic keratoses will eventually evolve into squamous cell carcinoma if left untreated. That might sound like a small percentage, but if you have a dozen on your face—and many people do—it adds up. Moreover, there’s no reliable way to predict which lesion will transform and which will stay dormant. It’s a bit like leaving rust spots on a car and hoping none of them will become a hole.
So, yes, you should care. Especially because treatment is usually quick, non-invasive, and highly effective if the lesion is caught early.
Common Questions People Ask (And Should Ask)
“If they’re so common, can I just ignore them?”
It’s tempting to dismiss them, especially when they’re asymptomatic. But AKs are more than cosmetic. They’re evidence that your skin has crossed a biological threshold—and that continued sun exposure may tip the balance toward malignancy. Ignoring them might work out for a while. It might also mean missing the early development of SCC, which is both avoidable and potentially disfiguring.
“What do dermatologists do about AKs?”
Fortunately, there’s a wide arsenal of treatments, and most are outpatient procedures with minimal downtime. The most common is cryotherapy—a quick freeze with liquid nitrogen that destroys abnormal cells. It stings, blisters slightly, and then heals. Other options include topical chemotherapeutics (like 5-fluorouracil or imiquimod), photodynamic therapy(where a photosensitizing agent is applied and activated with a specific light source), and chemical peels for broader field treatment. Your dermatologist will tailor the approach based on how many AKs you have, where they are, and how your skin reacts.
“Can AKs come back?”
Yes, and they often do. Treating an actinic keratosis doesn’t undo the UV damage in your skin—it simply removes a lesion that’s gone rogue. That’s why AKs are often part of what dermatologists call a “field cancerization” effect: a whole zone of sun-damaged skin with multiple unstable patches. This is why long-term prevention and surveillance are just as important as initial treatment.
“Is it really that big of a deal?”
If you care about your future self, yes. AKs are an early signpost of where your skin has been and where it might be headed. You might be able to live with one or two without consequence, but letting them accumulate unchecked is like letting mold spread behind drywall. You won’t see the full damage until it’s harder—and more expensive—to fix.
Don’t Panic—But Don’t Shrug It Off
Here’s the good news: if you’ve been diagnosed with actinic keratosis, you’re in a fortunate position. You’ve caught the problem before it turned into cancer. That gives you a head start. It’s an invitation to take your skin seriously—not with fear, but with respect.
And in a way, this is where sunspots and AKs start to overlap. Both are signs of sun damage. One is cosmetic; the other is precancerous. Both are preventable going forward.
In the next section, we’ll tie everything together by focusing on how to tell the difference between benign sunspots, precancerous AKs, and actual skin cancer. Because when you’re staring in the mirror, the skin doesn’t come with a label. You have to know what clues to look for—and that’s exactly what we’ll cover next.
Differentiating Sunspots from Skin Cancer
So now that we’ve walked through the big three—sunspots, skin cancer, and the often-overlooked actinic keratosis—you might be wondering: Okay, but how do I actually tell them apart? It’s a fair question, and it’s one that dermatologists wrestle with daily. The truth is, even for trained professionals, differentiating between these lesions isn’t always straightforward at first glance. That’s why dermatology leans so heavily on tools like dermoscopy, biopsies, and pattern recognition. But that doesn’t mean you’re helpless at home.
Let’s talk about what you can reasonably notice—and when it’s time to stop playing detective and call in the pros.
Appearance Isn’t Everything… But It’s a Start
When you’re scanning your skin, you’re not just looking for “bad” spots. You’re looking for change, difference, and inconsistency. But before we get to those red flags, let’s lay a visual foundation.
Sunspots are, by nature, pretty unremarkable. That’s part of why they fly under the radar. They tend to be:
- Flat and oval or round
- Light to dark brown (uniform in color)
- Smooth in texture
- Consistently shaped over time
- Located on areas with long-term sun exposure: cheeks, forehead, hands, shoulders
They don’t itch, they don’t bleed, and they don’t evolve. They show up, settle in, and stay put.
Actinic keratoses, in contrast, often feel wrong before they look wrong. You might rub your hand over your scalp or the side of your face and feel a little rough patch that you didn’t notice before. They tend to be:
- Rough or scaly to the touch
- Pinkish or reddish, sometimes crusty
- Tender or occasionally itchy
- Subtle, but persistent
Then there’s skin cancer, which plays by very different rules. Here’s the real trick: most cancers don’t look “bad”—they look different. Different from everything else on your skin. Different from what you remember being there last summer. And they tend to break the rules your other spots follow.
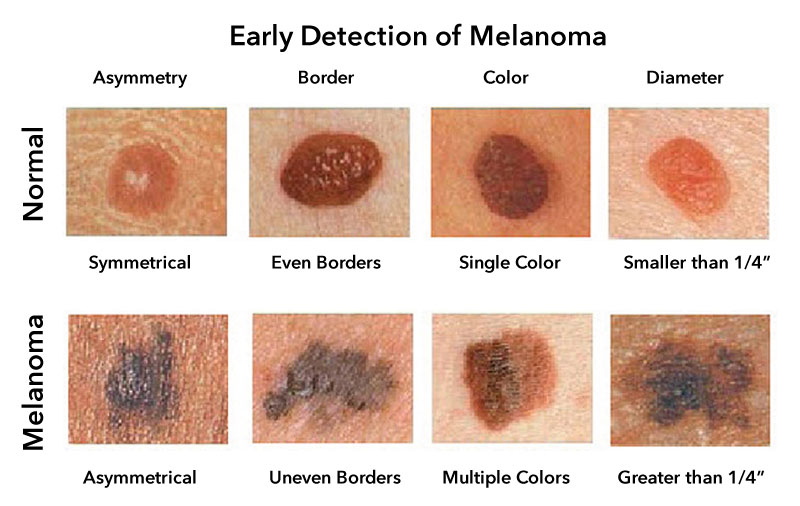
Enter the ABCDE Rule
One of the most powerful (and easy-to-remember) tools in early melanoma detection is the ABCDE rule. It’s not perfect, but it gives you a framework for evaluating whether a spot might warrant closer inspection.
- A is for Asymmetry: One half doesn’t match the other.
- B is for Border: Irregular, scalloped, or poorly defined edges.
- C is for Color: Multiple shades of brown, black, blue, red, or even white.
- D is for Diameter: Larger than 6mm (about the size of a pencil eraser), though smaller ones can be dangerous too.
- E is for Evolving: Changes in size, shape, color, elevation—or symptoms like itching or bleeding.
People often ask, Do I need to memorize this? Maybe not word-for-word, but internalize the spirit of it. You’re watching for outliers—spots that break the pattern of your own skin. The “ugly duckling” is another great rule of thumb: if you have a mole or spot that looks and behaves differently from all the others, that’s worth a second look.
Still Not Sure? That’s Normal.
One of the most frustrating aspects of skin self-monitoring is that things don’t always fit neatly into categories. You might find a brown patch that’s flat and harmless-looking… but it’s new. Or a rough area that hasn’t changed in months… but also hasn’t healed. This ambiguity is part of the reason dermatologists exist.
A good rule to live by: when in doubt, check it out. A quick office visit, a two-minute dermatoscope exam, or a simple biopsy can spare you months of anxiety—and possibly catch something serious early, while it’s still easily treatable.
It’s also worth noting that the skin doesn’t just develop one problem at a time. It’s entirely possible to have sunspots, actinic keratoses, and a small basal cell carcinoma all in the same area. That’s why a comprehensive skin exam looks at the entire picture, not just one isolated patch.
What You Can (and Can’t) Do at Home
Yes, you can keep an eye on your skin. Yes, you can photograph lesions every month or two to watch for changes. And yes, you can apply the ABCDE rule or feel for rough spots in high-risk areas.
What you shouldn’t do is fall into one of two extremes:
- Dismiss everything: “It’s probably just a freckle.” This can lead to dangerously late diagnoses.
- Obsess over everything: “This is definitely melanoma.” This fuels anxiety and usually leads to misinterpretation.
The truth is somewhere in the middle. Be proactive. Pay attention. But recognize the limits of what your bathroom mirror can tell you.
In the next section, we’ll walk through how skin lesions are actually diagnosed and monitored by professionals—from the moment you point one out to your doctor, to how it gets classified, to what the next steps usually look like. If you’ve ever wondered what exactly happens during a skin check or what to expect from a biopsy, you’ll want to stick around. This is where uncertainty begins to meet clarity.
Diagnosis and Monitoring
So let’s say you’ve found a spot. Maybe it’s new. Maybe it’s been there for years but seems… different. Or maybe it’s just nagging at your instincts, even though it looks pretty ordinary. What happens next? How do you go from “Hmm, that looks off” to actually knowing whether it’s benign, precancerous, or malignant?
This is where dermatology turns from educated guessing into something more methodical. Diagnosis and monitoring are not about panic, and they’re certainly not about playing skin whack-a-mole. It’s about gathering enough information to make an informed, evidence-based decision. And the process is actually more straightforward than most people think.
The Self-Check: Your First Line of Defense
Before we even get to the dermatologist’s office, let’s talk about what you can do yourself—because in most cases, youare the first person to notice when something on your skin changes. That puts you in a unique position of power.
No one’s suggesting you do a daily forensic analysis of your freckles, but a monthly or bimonthly check-in—especially if you’re over 40, fair-skinned, or have a history of sunburns—can make a real difference. This doesn’t have to be an ordeal. In fact, many dermatologists recommend doing it as part of a post-shower routine when your skin is clean, hydrated, and easy to examine under good lighting.
Use a full-length mirror and a handheld mirror, and make sure to check places people often forget: the scalp, the backs of the ears, underarms, soles of the feet, and under nails. You’re not trying to memorize every mark on your body; you’re just trying to notice what changes.
If something stands out—maybe it’s a new spot, maybe it’s an old one acting weird—write it down or take a photo. Having a personal skin record, even on your phone, is incredibly useful when it’s time to visit a professional.
What Happens During a Skin Exam?
Now you’ve booked your dermatology appointment. Great. So what’s going to happen?
A full-body skin exam is exactly what it sounds like. You’ll be asked to undress (usually down to your underwear), and the dermatologist will examine your skin from head to toe using both the naked eye and a dermatoscope—a handheld device with polarized light that allows a closer, more detailed look at structures beneath the surface of the skin.
Dermatologists aren’t just looking for “ugly” spots. They’re looking for asymmetry, border irregularity, color variation, vascular patterns, and any changes from your baseline. If they find something suspicious, they’ll decide whether it needs to be biopsied—or whether it’s safe to monitor.
And here’s the important part: not every concerning spot gets biopsied right away. Sometimes, the dermatologist will simply photograph it, make a note, and schedule a follow-up in 3 or 6 months. This is especially true for lesions that are borderline in appearance. Monitoring for change is often just as diagnostic as a biopsy.
Biopsy: It’s Not as Scary as You Think
People hear the word “biopsy” and assume the worst. But in dermatology, biopsies are a routine diagnostic tool, not a sign of impending doom.
There are several types of skin biopsies, and which one your doctor chooses depends on the size, depth, and suspected nature of the lesion:
- Shave biopsy: A superficial removal of the top layers of skin. This is quick and often doesn’t require stitches.
- Punch biopsy: Uses a small circular blade to take a full-thickness skin sample. Usually closed with one or two sutures.
- Excisional biopsy: Removes the entire lesion with some surrounding tissue. This is used when melanoma is strongly suspected or the whole spot needs to come out anyway.
The procedure typically takes 10–20 minutes, is done under local anesthesia, and you can walk out of the office and go about your day. The sample is then sent to a pathology lab, where a dermatopathologist examines it under a microscope to make the final call.
Waiting for Results: A Mental Game
This is the part patients often find hardest—not the biopsy itself, but the wait. It can take anywhere from a few days to a couple of weeks to get results, depending on the complexity of the case and the lab’s workflow.
During that time, it’s easy to fall into worst-case-scenario thinking. But here’s what you should know: most biopsied skin lesions turn out to be benign. Dermatologists have a low threshold for sampling anything even remotely suspicious, which is why so many “better safe than sorry” biopsies turn up nothing serious.
But when something is caught early—be it an actinic keratosis, a basal cell carcinoma, or even a melanoma—the odds are overwhelmingly in your favor. Treatment is more effective. Scars are smaller. And the long-term impact? Often negligible.
Monitoring Over Time
Let’s say everything comes back benign. That’s great news—but it doesn’t mean you’re off the hook forever.
Your dermatologist may recommend routine checkups every 6 to 12 months, especially if you’ve had a skin cancer before or have a significant history of sun exposure. This isn’t paranoia; it’s prevention. Remember, the same skin that produced one lesion is capable of producing others.
Monitoring also includes you, at home, continuing to stay aware of your skin’s normal patterns and reporting anything new or unusual promptly. The goal isn’t to make you neurotic—it’s to make you confident. You should know what’s normal for your body the same way you know your usual heartbeat or appetite. Skin health should be no different.
Treatment Modalities
Let’s say the biopsy came back, and this time it wasn’t nothing. Maybe it’s a basal cell carcinoma. Maybe it’s an actinic keratosis that’s starting to look suspicious. Or maybe it’s a melanoma that, thankfully, was caught early. You’ve got your diagnosis—but now what?
This is where things shift from worrying to doing. And contrary to the fear that often bubbles up around the word “cancer,” treatment for most skin lesions—benign, precancerous, or malignant—is highly effective, usually minimally invasive, and increasingly personalized. In other words, this is not the part where you should panic. This is the part where you get informed and start making calm, strategic decisions.
Treating Sunspots: Cosmetic, Not Medical
Let’s get the easy one out of the way first. If you’re dealing with a sunspot—and you’ve confirmed it’s just that—it’s not dangerous, and you technically don’t have to do anything. That said, if it bothers you cosmetically (and for many people it does, especially when they cluster on the face or hands), there are several ways to reduce or remove them.
Most dermatologists will start with non-invasive options like:
- Topical brightening agents, such as hydroquinone, retinoids, azelaic acid, or kojic acid, which help fade pigmentation over time.
- Laser therapy, which targets melanin with concentrated light to break up the pigment.
- Chemical peels, which exfoliate the surface layers of the skin, reducing sunspots while also improving texture and tone.
None of these treatments are one-and-done magic fixes. They often require a series of sessions, daily commitment, and sun protection going forward—because if new sun damage occurs, the spots will come right back.
Actinic Keratosis: Stop It Before It Starts
Because AKs are precancerous, they fall into a different treatment category: not cosmetic, but preventive. The goal here is to eliminate abnormal cells before they become invasive.
Treatment depends on how many lesions you have and where they are. For a few isolated spots, cryotherapy—that little burst of liquid nitrogen—is the go-to. It’s quick, precise, and usually doesn’t require numbing. The lesion blisters and peels off in about a week or two.
But if you’ve got a broader field of sun damage, topical therapies are often more appropriate:
- 5-fluorouracil (5-FU): A topical chemotherapy cream that causes sun-damaged skin to slough off. It’s messy, uncomfortable, and a little unsightly during treatment—but highly effective.
- Imiquimod: An immune response modifier that stimulates your body to attack abnormal cells.
- Photodynamic therapy (PDT): A two-step process where a light-sensitizing solution is applied, followed by a blue or red light to activate it. Think of it as high-tech spot cleaning.
Each of these has trade-offs in terms of downtime, visibility, and side effects, but the bottom line is: AKs are treatable, and treating them early is a smart, proactive move.
Basal and Squamous Cell Carcinoma: Local, But Not Low Priority
When it comes to BCC and SCC, the most common approach is surgical—and for good reason. These cancers, while rarely life-threatening, can be locally aggressive. They don’t just sit on the surface; they dig. So the goal is to remove them completely, and to do so in a way that minimizes the risk of recurrence.
The most common methods include:
- Excisional surgery: This is what it sounds like—the lesion is cut out with a margin of healthy tissue. It’s sent to the lab to ensure clean edges, and you’re stitched up in a tidy little arc. Simple, effective, and often done in-office.
- Mohs micrographic surgery: This is the gold standard for high-risk areas like the face, ears, or hands. It involves removing the lesion layer by layer while examining each under a microscope until no cancerous cells remain. It preserves the most healthy tissue and offers the highest cure rate—especially important for cosmetically sensitive areas.
- Curettage and electrodesiccation: Often used for superficial BCCs or early SCCs. The lesion is scraped off, and the base is cauterized. Quick, but not typically used for deeper or more aggressive cancers.
Some early lesions can also be treated non-surgically, especially in patients who aren’t good candidates for excision:
- Topical treatments like 5-FU or imiquimod (yes, again—they pull double duty here).
- Radiation therapy, reserved for elderly patients or those with larger lesions in difficult-to-operate regions.
The key? Tailoring treatment to the patient’s needs, the cancer’s behavior, and the anatomical context.
Melanoma: The One That Demands Precision
Melanoma is in a class of its own. Unlike BCC and SCC, it has real metastatic potential. That means treatment isn’t just about removing the lesion—it’s about making sure it hasn’t spread, and preventing it from doing so.
- Wide local excision is the first step. The lesion is removed with a larger margin (often 1–2 cm) to ensure all malignant cells are gone.
- Sentinel lymph node biopsy may be performed if the melanoma is deep enough (usually >1mm thick), to check for regional spread.
- If lymph nodes are positive, or the melanoma is advanced, treatment may escalate to immunotherapy or targeted therapy—a whole new class of drugs designed to boost the immune system or disrupt specific genetic mutations driving the cancer.
It’s worth noting: melanoma caught early is almost always curable with surgery alone. That’s why early detection is everything.
What About Scarring?
It’s a common question—and a reasonable one. Yes, most treatments for precancerous or cancerous lesions will leave some kind of mark. But skilled dermatologic surgeons are also artists, especially when it comes to facial work. Incisions are made along natural skin lines, sutures are placed to minimize tension, and post-op care can significantly reduce scarring.
And here’s the bigger truth: a small scar is a much better outcome than an untreated cancer. In the tradeoff between aesthetics and safety, you don’t have to completely sacrifice one to achieve the other.
Choosing the Right Treatment Isn’t a Solo Act
You don’t have to make these decisions alone. Dermatologists will guide you, explain your options, and help you choose a path that fits your medical needs, lifestyle, and preferences. There’s rarely only one “correct” treatment—there’s a spectrum of choices, each with pros and cons. Your job is to be informed, ask questions, and show up for your skin. Their job is to bring the science and the surgical skill.
Prevention Strategies
At this point, you might be thinking, All right, I get it—sun damage is real, cancer is a risk, but is there anything I can actually do about it now? The answer is an emphatic yes. In fact, if there’s a silver lining to everything we’ve discussed so far, it’s this: most of it is preventable. Not guaranteed, not foolproof—but highly modifiable.
Skin cancer isn’t a fate sealed by genetics or geography. It’s largely a disease of cumulative exposure—years of UV radiation slowly wearing down your skin’s natural defenses. And while you can’t go back and undo that week in Cancun when you didn’t reapply sunscreen once, what you do from this point forward can make a dramatic difference.
Sun Protection: Yes, It’s Still That Important
Let’s start with the obvious but still-too-often-ignored advice: wear sunscreen. And not just when you’re heading to the beach. UV radiation doesn’t care if you’re gardening, walking to lunch, or driving in your car (yes, UVA rays go right through glass). The real game-changer is consistency. Daily application of broad-spectrum SPF 30 or higher—even on cloudy days—is the single best way to reduce your risk of sunspots, actinic keratoses, and skin cancer.
This isn’t just theoretical. Multiple longitudinal studies have shown that people who use sunscreen daily significantly reduce their rate of new actinic keratoses and non-melanoma skin cancers. It’s one of the rare cases in medicine where the return on investment is both immediate (fewer sunspots) and long-term (less risk of cancer).
And no, sunscreen is not all the same. Look for:
- Broad-spectrum coverage (protects against both UVA and UVB)
- Water resistance if you’re sweating or swimming
- Physical blockers like zinc oxide or titanium dioxide if you have sensitive or acne-prone skin
But even sunscreen isn’t a force field. It’s a tool—one part of a broader strategy.
Don’t Just Block the Sun—Outsmart It
Sun protection also means changing your relationship with sunlight, not avoiding it altogether, but learning how to be in it without paying the price.
Here’s what that might look like:
- Seek shade between 10 a.m. and 4 p.m., when UVB rays are strongest. Even 30 minutes less exposure during peak hours can reduce cumulative damage.
- Wear protective clothing: lightweight, long-sleeved shirts; wide-brimmed hats; and UV-blocking sunglasses aren’t just for outdoor workers and desert hikers. They’re your everyday armor.
- Get to know the UV Index: It’s updated daily in most weather apps and tells you how strong the sun’s rays are in your area. Anything over 3 means precautions are a good idea. Over 6? Get serious.
This isn’t about paranoia—it’s about strategy. A few habit changes can help your skin age more gracefully and lower your cancer risk substantially.
Ditch the Tanning Bed—Completely
This one should go without saying, but let’s say it anyway: tanning beds are a carcinogen. They are literally classified by the World Health Organization as Group 1, alongside tobacco and asbestos. And no, using them “occasionally” doesn’t make them safer. Just one indoor tanning session before the age of 35 increases your melanoma risk by nearly 60%. That’s not a typo.
If you love the look of bronzed skin, opt for sunless tanning products. There are excellent self-tanners and professional spray options out there that give you the glow without mutating your melanocytes.
Think Long-Term, Not Just Summer
One of the reasons people fall off the sun protection wagon is that they treat it like a seasonal chore. But skin cancer doesn’t care what month it is. UVA rays, in particular, are present year-round and penetrate through clouds and glass. That’s why the winter vacation to the mountains—or the daily drive in your car—can be just as damaging as a beach trip in July.
Consistency is what matters. Building sun protection into your daily routine (apply sunscreen after brushing your teeth, keep a hat in the car, reapply at lunchtime) turns it from a chore into muscle memory.
Prevention Also Means Screening
Let’s not forget: even if you’ve been a sun protection saint your whole life, screening still matters. Skin changes naturally as you age, and not every skin cancer is caused by UV light (some are driven by genetics, immune suppression, or viral infections like HPV).
Regular skin checks—both self-exams and professional evaluations—are your early-warning system. If you’re high risk (fair skin, family history, history of sunburns, personal history of skin cancer), annual dermatology visits are a wise investment. For others, every 1–2 years may suffice. It’s not about fear—it’s about early detection. And early detection is often the difference between a minor outpatient procedure and something far more invasive.
Is It Ever Too Late to Start Protecting Your Skin?
Absolutely not. This is a question patients ask all the time, often with a guilty look: “I never wore sunscreen growing up—does it even matter now?”
Yes, it matters. Your skin is dynamic and resilient. While past damage can’t be erased, future damage can absolutely be minimized. Starting sun protection in your 40s, 50s, or beyond still helps. It lowers your risk of new sunspots and cancers, and it gives your skin a fighting chance to heal and regulate itself better.
Psychological and Social Considerations
Skin cancer, sun damage, suspicious lesions—on paper, these sound like purely physical concerns. Cells misbehaving, UV rays misfiring, DNA repair mechanisms faltering. But let’s be honest: that’s not the whole story. We don’t experience skin conditions as abstract biology. We live them. We see them in the mirror. We feel them every time someone asks, “What’s that on your cheek?” or when a biopsy scar on our nose changes the way we smile in photos.
Skin issues—especially those involving cancer or the possibility of it—can provoke not just medical anxiety, but real emotional weight. And that’s a part of the story that deserves just as much space as the clinical facts.
Appearance Isn’t Vanity—It’s Identity
Let’s start with something a lot of people feel but hesitate to say: it’s okay to care about how your skin looks. That doesn’t make you vain or superficial. It makes you human. Skin is the most visible part of us. It’s our interface with the world, and when something about it changes—whether it’s a lesion, a scar, a rash, or post-treatment discoloration—it can shake your sense of self.
Patients often say things like, “I know I shouldn’t care—it’s just cosmetic,” especially after a skin cancer excision on the face. But that’s a false dichotomy. You can care deeply about your health and about your appearance. And when those two domains collide, it’s normal to grieve the loss of how things used to look, even while being grateful for catching something early or for surviving it.
This is especially true when treatments leave visible marks—on the nose, forehead, or cheek. It can be hard to celebrate being “cancer-free” when your reflection feels like a reminder of what you went through.
So let’s normalize this: appearance matters. Not more than health, but not less than it either. Your emotional response to visible changes is valid, and acknowledging that doesn’t make you any less strong or resilient.
Fear, Shame, and the “What If” Spiral
There’s also the mental load that comes before diagnosis. The waiting. The guessing. The endless Googling and the quiet voice in your head asking, What if it’s melanoma? What if I waited too long?
This anticipatory anxiety is common. It’s especially brutal in the days between a skin check and the biopsy results. You might feel fine, but your brain has already played out every worst-case scenario. You imagine phone calls with your family. You picture hospital rooms that may never materialize. And all the while, you’re trying to hold it together at work or during school drop-off.
And when the results come back benign? Relief, sure. But also a strange kind of guilt—Was I overreacting? Was I being dramatic?
You weren’t. You were being proactive. And if it had been something serious, you would’ve been prepared. That kind of engagement with your health isn’t paranoia—it’s wisdom in action.
Navigating Conversations with Others
Then there’s the social side of this. Not everyone in your life will know how to talk about skin cancer, or skin damage, or even actinic keratoses. Some people will say all the right things. Others will brush it off: “Oh, it’s just skin stuff, no big deal.”
The truth is, it is a big deal. Maybe not because it’s life-threatening (although it can be), but because it forces you to confront your vulnerability in a very visible, public way. Especially if you’ve had surgery, or you’re undergoing topical treatment that makes your skin red, peeling, or crusted. You don’t get to hide that. It’s there when you check out at the grocery store. It’s there when you’re on Zoom calls.
If you’ve ever felt like you had to explain yourself before anyone even asked—“It’s a treatment for pre-cancer, I’m okay, it just looks bad for now”—you’re not alone. The visibility of these treatments can trigger self-consciousness, even among the most confident people. And that can lead to social withdrawal, altered self-esteem, even depression if left unacknowledged.
Coping Strategies That Actually Work
So how do you manage all this? It’s not about suppressing the discomfort—it’s about supporting yourself through it.
- Talk to someone, whether that’s a friend, a partner, or a therapist. Saying out loud what you’re feeling helps demystify it—and puts emotional distance between you and the anxiety.
- Give yourself permission to be bothered by the visible stuff. You don’t have to pretend it’s fine if it’s not. Healing isn’t just about closing wounds; it’s about integrating the experience.
- Ask your dermatologist about scar-minimizing techniques before and after treatment. Knowing you have options—even small ones—restores a sense of control.
- Join a community. Online forums or local support groups for skin cancer patients and survivors can be grounding. Not because misery loves company, but because shared experiences dissolve shame.
And perhaps most importantly: reframe the narrative. That scar isn’t just a blemish—it’s proof that you paid attention, acted early, and made your health a priority. Over time, that can become a source of pride rather than regret.
The Psychological Payoff of Prevention
There’s one more point worth making: prevention isn’t just physically protective—it’s mentally freeing. When you know you’re doing your part—applying sunscreen, checking your skin, showing up for annual exams—you quiet that anxious little voice that says, What if I missed something?
Prevention puts you on offense, not defense. It turns fear into stewardship.
In the next section, we’ll zoom out a bit and look at some of the cutting-edge research happening in dermatology and oncology: how diagnostic tools are evolving, what treatments are on the horizon, and where science is heading in the ongoing fight against skin cancer. Because even as individuals do their part, the medical world is moving too—and some of those changes are quietly revolutionary.
Frequently Asked Questions (FAQs)
1. Do sunspots increase my risk of skin cancer?
Sunspots themselves (solar lentigines) are not precancerous and won’t turn into skin cancer. But their presence signals cumulative sun damage — the very thing that does raise your skin cancer risk. Think of them as a warning light: harmless in isolation, but part of a bigger picture that calls for regular skin exams and diligent sun protection.
2. How can I tell if a spot is benign, precancerous, or dangerous?
Sunspots tend to be flat, evenly colored, and stable. Actinic keratoses, on the other hand, are often rough, scaly, and reddish, and they may come and go. Skin cancers break the rules — they may itch, bleed, evolve, or just look “off.” If something changes or seems different from the rest, a dermatologist should take a look. When in doubt, check it out.
3. Can people with darker skin get sun damage or skin cancer?
Yes — absolutely. While darker skin contains more melanin, which offers some protection, it doesn’t make you immune. In fact, skin cancers in people with darker skin are often detected later and may be more serious. Everyone benefits from sun awareness, regardless of skin tone.
4. What should I do if a mole or spot changes, itches, or bleeds?
Any change in size, shape, color, or behavior — including itching, bleeding, or crusting — is a red flag. Don’t wait and see; early evaluation can make all the difference. Even “normal-looking” spots can harbor hidden risk if they start acting differently.
5. Can sun-damaged spots be removed — and will they come back?
Yes, many sunspots can be lightened or removed with treatments like peels, lasers, or topicals. Actinic keratoses can be cleared with freezing or medications. But unless you limit sun exposure going forward, these spots (and new ones) may return. Sun protection is what makes the difference long term.
6. How can I protect my skin and lower my cancer risk going forward?
Daily sunscreen use is a powerful cancer-prevention tool, not just a sunburn shield. There’s no miracle supplement, but a healthy diet may help support skin repair. Most importantly, see a professional annually (or more often if you’ve had skin cancer before) and perform self-checks at home. It’s never too late to start — your skin will thank you.
Closing Thoughts
If you’ve read this far, you’re already ahead of the game. The reality is, most people don’t give their skin much thought until something changes—or worse, something goes wrong. But the truth is, skin health is an ongoing relationship, not a one-time crisis to manage. Sunspots, actinic keratoses, and skin cancers are all part of the same spectrum: the visible effects of a life lived under the sun. Knowing how to read those signs—not with fear, but with curiosity and respect—is empowering.
You don’t have to obsess, and you don’t have to live in the shade. You just need to be proactive. That means embracing sunscreen, building sun-smart habits, and knowing your skin’s patterns as intimately as you know your smile or your voice. It means seeing a dermatologist not out of panic, but out of self-care. And above all, it means recognizing that health and appearance can, and should, coexist.
Remember: your skin is talking to you. Sometimes it whispers. Sometimes it shouts. The more fluently you learn its language, the better you’ll be able to protect it, treat it, and—most importantly—enjoy it.
Here’s to taking care of the skin you’re in, for life.



