Supplements for Dogs with Cancer | Full Guide for Pet Owners
- Foreword
- Part 1: Understanding Canine Cancer
- Part 2: The Role of Nutrition in Canine Cancer Care
- Part 3: Overview of Supplements for Dogs with Cancer
- Part 4: Categories of Beneficial Supplements
- Part 5: Selecting Quality Supplements — What to Look For and What to Avoid
- Part 6: Monitoring and Adjusting Supplement Use — Staying Responsive to Your Dog’s Needs
- Part 7: Case Studies and Testimonials — Real Stories, Real Insights
- Part 8: Frequently Asked Questions (FAQ)
- Closing Thoughts
Foreword
When a beloved dog is diagnosed with cancer, it’s as if the world shifts on its axis. You might remember the exact moment the vet said the word. It hits hard. The diagnosis brings not only emotional upheaval but a torrent of questions: “What are my options? How do I give my dog the best quality of life now? What more can I do?”
Among the options explored by many pet owners—often after long hours of research and difficult conversations—is the idea of supplements. You’ve likely seen claims about turmeric reducing inflammation, mushroom blends boosting the immune system, or CBD helping manage pain and anxiety. The space is noisy. The stakes are high. And what your dog needs most right now is clarity and care, not marketing gimmicks.
This article was created to be your final stop in that search. Not because it claims to have all the answers, but because it brings together everything that is known—from veterinary science to integrative therapies to real-world experience. It’s grounded in compassion, but guided by rigor.
Our goal is to help you understand what supplements can (and can’t) do for a dog with cancer, how to make thoughtful choices in collaboration with your vet, and what to watch for along the way. We’ll also address the big-picture context: how cancer affects your dog’s body, how diet and environment factor in, and where supplements fit into a wider care plan.
So let’s start at the root of the issue. Because before we talk about what to give your dog, we need to talk about what they’re up against.
Understanding Canine Cancer
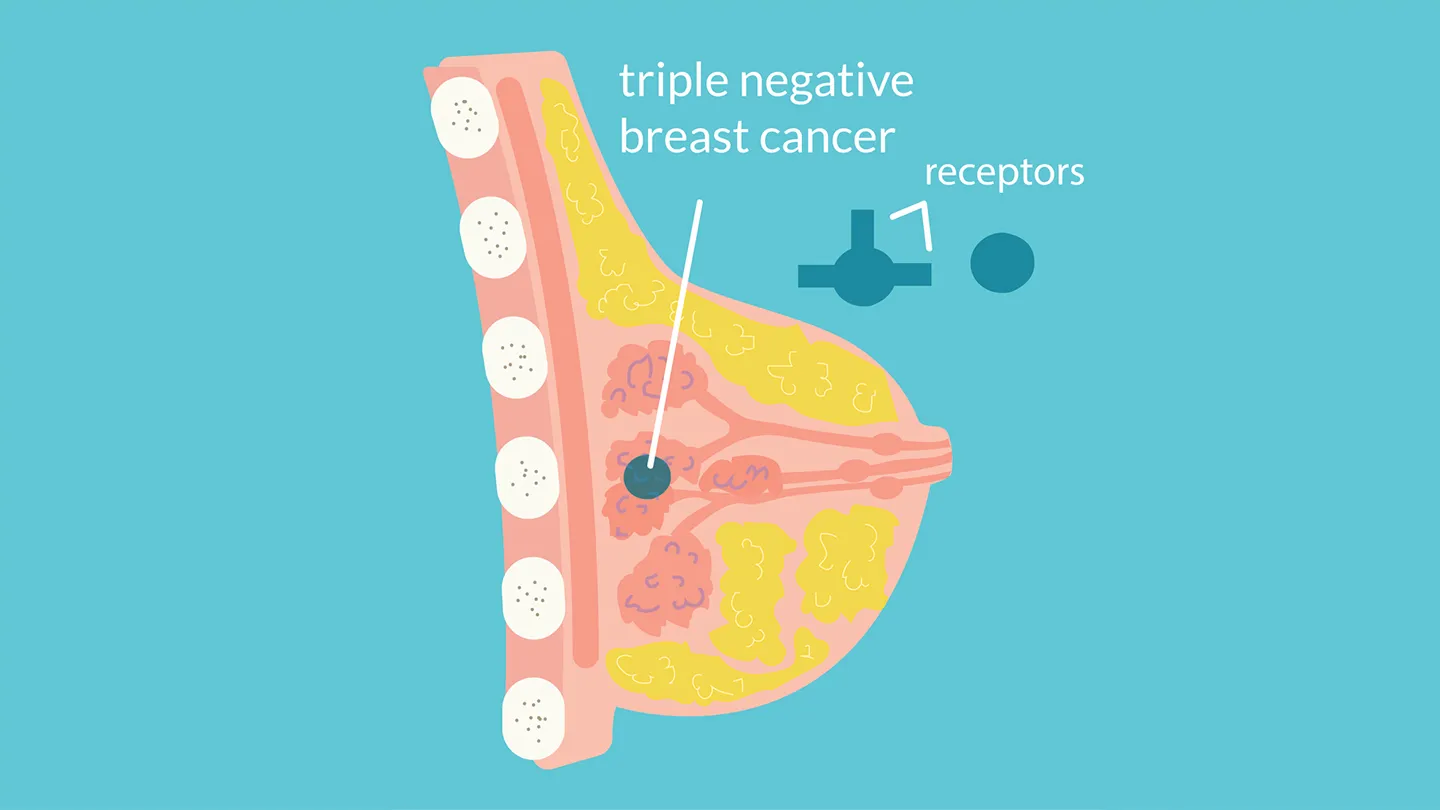
What exactly is cancer in dogs?
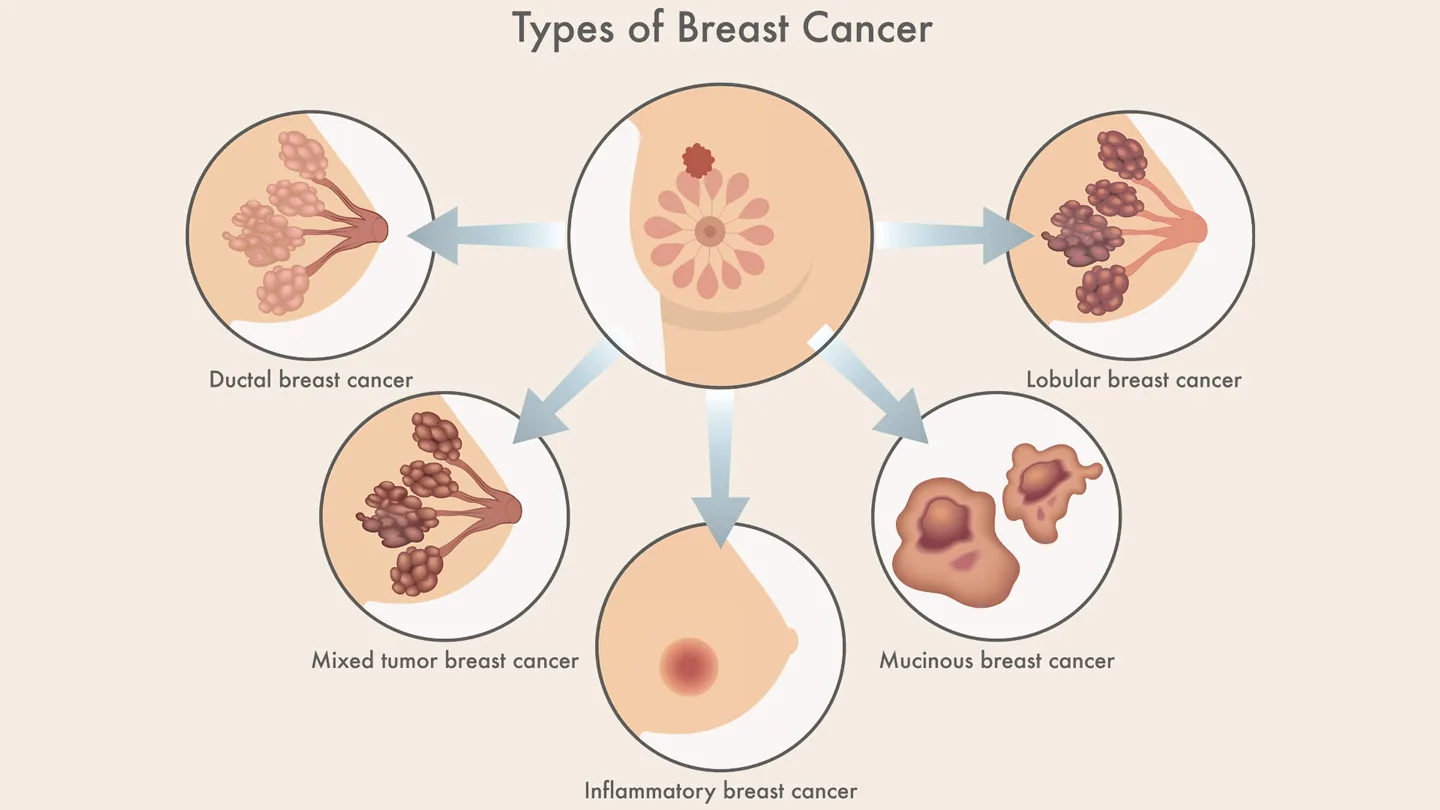
Cancer isn’t a single disease—it’s a catch-all term for a group of conditions where cells grow uncontrollably, often forming tumors or invading other tissues. It’s surprisingly common in dogs. In fact, cancer is the leading cause of deathin older dogs, and some breeds—like Golden Retrievers, Boxers, and Bernese Mountain Dogs—have significantly higher rates due to genetic predispositions.

But let’s pause here: What does “cancer” really mean for your dog?
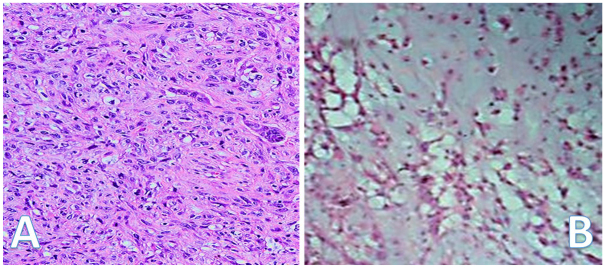
It could be a mast cell tumor on the skin, a lymphoma affecting the immune system, or a hemangiosarcoma, a stealthy blood vessel cancer that often goes unnoticed until it’s advanced. Some cancers grow slowly; others are devastatingly aggressive. Each type behaves differently, which is why a correct diagnosis—including biopsy and staging—is crucial to any treatment plan.
What causes cancer in dogs?
Here’s the short answer: it’s complicated.
Cancer arises from a mix of genetics, environmental exposure, and lifestyle factors. Some dogs are born with genetic mutations that make cancer more likely. But environmental toxins—like lawn chemicals, secondhand smoke, and even some commercial dog foods—can also play a role. And while we don’t yet understand all the connections, there’s increasing interest in how chronic inflammation and oxidative stress contribute to cancer’s development and progression.
Is there something I could’ve done to prevent it?
That’s a question most pet owners ask themselves. It’s also one of the hardest to answer. While it’s true that some cancers can be influenced by external factors (diet, toxins, spay/neuter timing), many develop without any clear cause. Blame doesn’t belong in the equation—support does. The most constructive step now is to focus on what you can control moving forward.
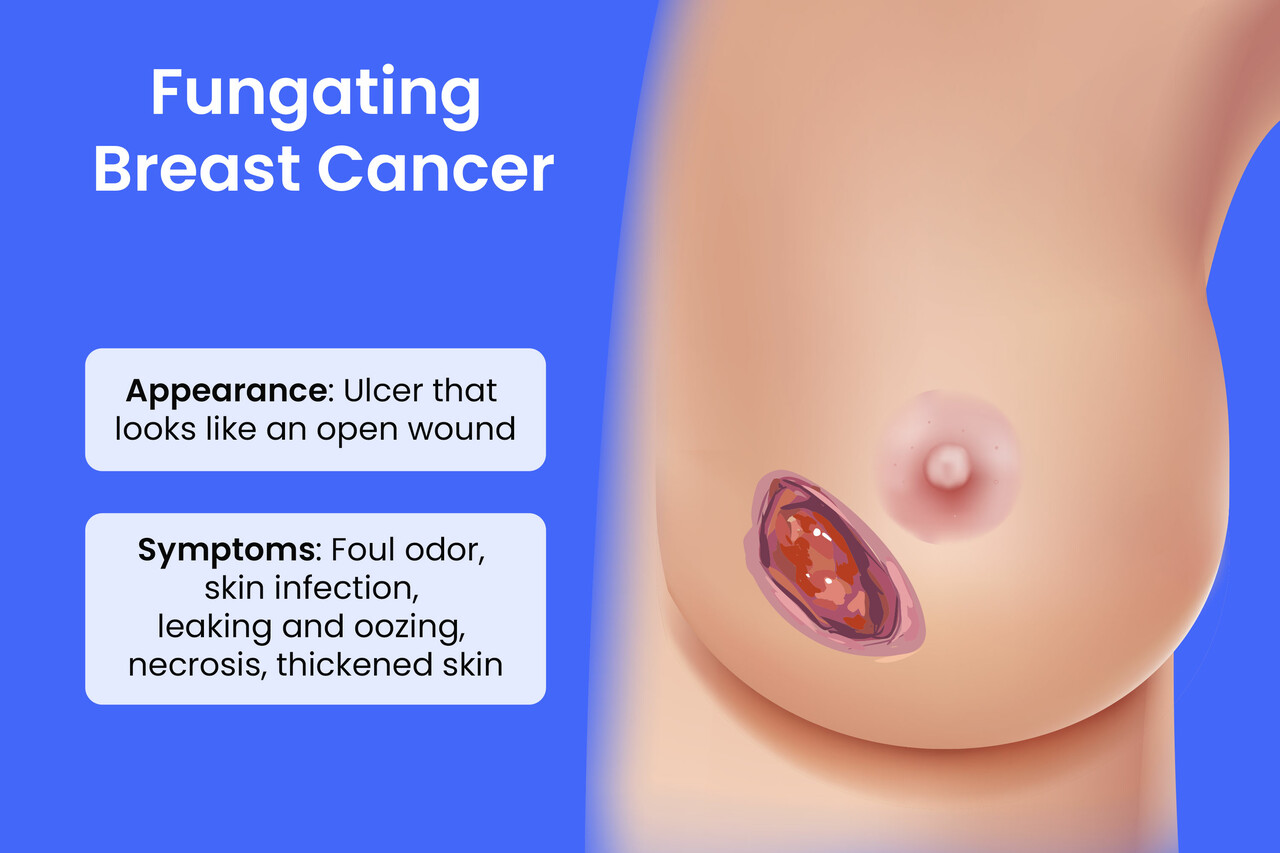
What signs should I have looked for—and what happens next?
Cancer in dogs doesn’t always announce itself clearly. Sometimes it’s a lump under the skin. Other times, it’s subtle: weight loss, fatigue, loss of appetite, unusual bleeding, or persistent coughing. If your dog is acting “off” for more than a few days, a vet visit is always the right call.

Once cancer is suspected, your vet may perform blood work, X-rays, ultrasounds, or tissue biopsies to identify the cancer type and determine how far it has spread. That’s called staging, and it’s critical for designing a treatment plan. This is also the point where you’ll begin to explore your options: surgery, chemotherapy, radiation, palliative care—and yes, nutritional support and supplementation.
But that brings us to the bigger picture: how does cancer affect a dog’s body over time, and how can nutrition play a role in fighting back?
Whether you’re navigating canine cancer for the first time or looking to complement treatment, Mouth Cancer in Cats shares a similarly emotional and practical care path.
That’s where we’re headed next. Because supplements don’t exist in a vacuum. They are part of a larger system—one that we can, and should, try to influence for the better.
The Role of Nutrition in Canine Cancer Care
You might be wondering: Can something as basic as food really make a difference in cancer care? It’s a fair question—especially when we’re so used to thinking about treatment in terms of surgery, chemotherapy, or radiation. But here’s the thing: nutrition is not just complementary to conventional cancer treatments—it can be foundational.

Let’s break it down. When a dog has cancer, the disease doesn’t just stay in a neat little corner of the body. It changes everything. It rewires metabolism, suppresses immune function, triggers inflammation, and can even rob the body of its ability to properly use nutrients. That’s why dogs with cancer often lose weight even when they’re eating, and why some experience sudden fatigue, infections, or gut issues that weren’t there before.
So yes, food matters. And the right nutrition can do more than sustain—it can strengthen, soothe, and support the body’s fight against cancer.
Diet as Medicine—Not a Buzzword
You may have heard about “cancer diets” for dogs. These often center on high-protein, low-carbohydrate formulations, and for good reason. Many cancer cells rely heavily on glucose (sugar) for energy. By reducing carbohydrate intake, the goal is to starve the cancer cells without starving the dog.
But this isn’t a matter of simply cutting carbs. You’re feeding a body in crisis—a body that needs easy-to-digest proteins, anti-inflammatory fats, and cell-protective micronutrients. So rather than “going keto” for your dog (a trend that’s oversimplified and often misapplied), the smarter move is to work with a veterinary nutritionist or an oncologist who understands the metabolic demands of cancer.
And don’t forget: treatment itself can wreck appetite. Some dogs will lose interest in food altogether. Others might only eat if hand-fed or coaxed with warming and aroma. Nutritional care has to be practical, not just theoretical.
What Should a Cancer-Friendly Diet Include?
There’s no one-size-fits-all formula, but certain nutritional themes have emerged from both research and real-world clinical practice:
1. High-quality protein
Muscle wasting (cachexia) is a real threat in canine cancer patients. Protein helps preserve lean tissue and supports immune repair. Think pasture-raised meats, organ meats, or hydrolyzed protein sources for dogs with sensitivities.
2. Healthy fats, especially omega-3s
Fats are calorie-dense (helpful for dogs with low appetite) and have potent anti-inflammatory effects. Omega-3s from fish oil (EPA and DHA specifically) have been shown to slow tumor growth in some models and support immune modulation.
3. Complex nutrients, not just calories
Your dog’s immune system needs zinc, selenium, vitamins A, D, and E, and a host of other cofactors to function optimally. That doesn’t mean megadosing—it means ensuring a nutrient-dense diet, ideally through whole foods or professionally designed formulations.
4. Low to moderate carbohydrates
While carbs aren’t inherently bad, the type and quantity matter. Avoiding high-glycemic, heavily processed grains is a sound strategy. Sweet potatoes, squash, and blueberries? Better choices, in moderation.
5. Digestive support
Cancer and chemotherapy can destabilize gut flora. A dog’s digestive tract is its largest immune organ. Supporting it with prebiotics, probiotics, and digestive enzymes can reduce inflammation and improve nutrient uptake.
Foods to Be Cautious About
Even with the best intentions, some common items in commercial diets or “natural” recipes can backfire. Highly processed kibble with artificial preservatives? Hard pass. Grapes, onions, xylitol, and certain mushrooms? Toxic. And while garlic gets praised in holistic circles, it’s best avoided in therapeutic doses unless under direct veterinary supervision—it can be harmful in excess.
The rule of thumb: if it’s powerful enough to help, it’s powerful enough to hurt when misused. That’s why we’re going to talk extensively about supplements soon. But before we get there, ask yourself this:
What is the goal of my dog’s nutritional support? Are you trying to slow cancer growth? Enhance recovery after chemo? Ease inflammation or digestive upset? Improve energy? These questions matter—because they’ll guide how you use food and supplements as tools, not just placeholders.
Can Diet Alone Treat Cancer?
No—and anyone who tells you otherwise is either misinformed or misleading you. Cancer in dogs is complex and stubborn. Nutrition is not a cure, but it is a powerful lever for improving resilience, minimizing side effects, and sometimes even extending survival time. More importantly, it improves quality of life—and in palliative cases, that’s the main battle worth fighting.
Some studies show that dogs on specific therapeutic diets live longer than their counterparts on conventional food. But again, results vary widely, and diet must be tailored.
The bottom line: if your dog has cancer, they deserve a diet that’s thoughtfully constructed—not just to feed the body, but to fortify it.
And once the foundation of nutrition is solid, that’s when supplements come in—targeted, precise, and evidence-based. In the next section, we’ll explore exactly what they are, what roles they play, and how to choose wisely in a market that’s equal parts promising and perplexing.
Overview of Supplements for Dogs with Cancer
Let’s start with a brutally honest question:
Are supplements for dogs with cancer worth it—or are they just hope in a bottle?
The answer is both simple and complex. Yes, some supplements are backed by credible research and clinical use. Yes, they can support your dog’s immune system, reduce inflammation, aid digestion, and even help mitigate side effects from chemo or radiation. But no, they are not miracle cures. And no, not all supplements are created equal—some are helpful, others are snake oil dressed up in a natural label.

In other words, supplements can be supportive—sometimes even transformative—but they are not a substitute for medical care. They are part of a broader care strategy, not a standalone solution. That’s where their true power lies: in synergy.
Why Use Supplements in Canine Cancer Care?
Let’s go deeper. What do we really expect a supplement to do for a dog with cancer?
There are several potential roles they can play:
1. Immune system support
Cancer suppresses immune function. Some supplements aim to restore or enhance it—especially important if your dog is undergoing chemo or radiation, both of which can further weaken immune defenses.
2. Anti-inflammatory action
Chronic inflammation is a hallmark of cancer—and of the damage it does to healthy tissues. Reducing this inflammation (without resorting to long-term steroids) is one of the most strategic interventions you can make.
3. Antioxidant defense
Cancer, treatment side effects, and even normal aging all generate oxidative stress. Some supplements may help neutralize the damage from free radicals, preserving cellular health.
4. Metabolic modulation
Some advanced supplements aim to starve tumors of fuel (glucose), or support mitochondrial function in healthy cells. This is still a newer frontier, but one that’s gaining traction, especially in integrative oncology.
5. Symptom and side-effect management
This includes everything from improving appetite to easing nausea, anxiety, pain, or diarrhea—symptoms that erode quality of life if left unaddressed.
But wait—shouldn’t my vet already be doing all this?
Good question. And in many cases, they are—at least partially. But most traditional veterinary oncologists focus on evidence-based conventional treatment: surgery, chemo, radiation, pain management. They may not be trained in nutritional science or integrative medicine, which is why collaborating with a vet who understands both sides of the coin can be invaluable.
This doesn’t mean going rogue with an all-natural protocol. It means building a team. Your dog’s oncologist may not recommend turmeric or medicinal mushrooms, but they also may not object if you ask about them intelligently, with data in hand and a clear goal in mind.
That’s the kind of conversation we want to empower you to have.
What Are the Risks of Using Supplements?
Now for a dose of necessary caution: just because it’s natural doesn’t mean it’s harmless. This is especially true when your dog is undergoing chemotherapy or taking other medications. Some supplements interact with drugs. Others can overwhelm the liver or kidneys if dosed incorrectly.
Here are a few watch-outs:
- Over-supplementation: More isn’t always better. Mega-doses of antioxidants, for instance, can sometimes interfere with the oxidative stress that chemotherapy uses to kill cancer cells.
- Contaminants: The supplement industry is underregulated. Some products contain heavy metals, fillers, or ingredients that aren’t even listed on the label.
- Wrong diagnosis, wrong support: Giving immune-boosting supplements to a dog with immune-cell cancer (like lymphoma) may backfire, depending on the mechanism.
This is why every supplement should be vetted—by your vet.
So… Where Do I Start?
If you’re thinking, “This sounds like a lot to figure out,”—you’re absolutely right. The goal here isn’t to overwhelm you, but to make you an informed, confident participant in your dog’s care.
In the next section, we’ll break down the major categories of supplements—what they do, which ones are most relevant for dogs with cancer, and how to distinguish the helpful from the hype. But for now, here’s what to take away:
- Supplements are tools. They are not cures, not crutches, but instruments that—when chosen carefully—can improve outcomes and ease suffering.
- Your dog’s biology is unique. What works for one dog with osteosarcoma may not work for another with lymphoma. Personalization is key.
- Your instincts matter. If something feels off, or too good to be true, pause. Bring it to your vet. Do more research. That’s not skepticism—it’s wisdom.
Next, we’ll dive into the actual categories of supplements: from immune modulators to anti-inflammatory agents, from antioxidants to digestive support—and everything in between. You’ll learn what the research says, what real-world results show, and what to watch out for when selecting products in an unregulated market.
There’s also a spotlight on emerging methods like Hyperthermia in Dogs with Breast Cancer, which you might consider alongside supplements.
Because this is your dog’s body. This is your battle, too. And you deserve nothing less than the whole truth.
Categories of Beneficial Supplements
Here’s where the rubber meets the road. You’ve made the decision to explore supplements for your dog with cancer—now the next question is: Which ones actually help?
The supplement aisle, whether online or at the local pet store, can be dizzying. Mushroom extracts, omega oils, turmeric chews, probiotics, herbal tinctures… they all come wrapped in promises. “Boosts immunity!” “Fights tumors!” “Supports longevity!” But beneath those glossy labels is a mix of science, tradition, marketing—and sometimes misinformation.
So let’s sort it all out. Below is a deep dive into the key categories of supplements used in integrative canine cancer care. This isn’t a shopping list—it’s a framework. Each category serves a different purpose, and not every dog needs something from each bucket. The goal isn’t to load your dog up with every “cancer-fighting” substance on the market. The goal is precision, balance, and evidence-backed decision-making.
Immune System Support
Let’s start with the immune system. It’s your dog’s natural surveillance system, constantly scanning for threats—including cancer cells. But cancer is sneaky. It evolves ways to hide, suppress, or hijack immune responses. That’s why immune support is such a critical—and popular—focus.
Medicinal Mushrooms (Turkey Tail, Reishi, Shiitake, Maitake)
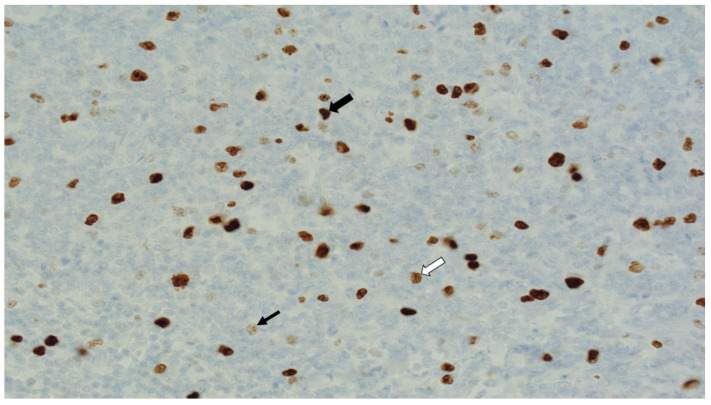
These are not your average grocery store mushrooms. Medicinal mushrooms contain compounds called beta-glucans, which stimulate immune cells like macrophages and natural killer (NK) cells.
Turkey Tail (Coriolus versicolor), in particular, has been studied in dogs with hemangiosarcoma—a notoriously aggressive cancer—and showed promising improvements in survival times. Is it a cure? No. But it may help tip the odds, especially when used alongside standard treatments.
Beta-Glucan Complexes
Even outside mushrooms, beta-glucans can be isolated and concentrated into supplements. They don’t attack cancer directly, but instead prime the immune system to respond more effectively. Think of them as enhancing the radar, not firing the missiles.
Are these safe? Generally yes, but immune-stimulating supplements should be used with caution in dogs with blood cancers like lymphoma or leukemia—where stimulating the immune system might unintentionally fuel the fire.
Anti-Inflammatory Agents
Cancer and inflammation are close companions. In fact, some scientists refer to tumors as “wounds that never heal.” So targeting inflammation can reduce pain, fatigue, tissue damage, and possibly even slow tumor progression.
Omega-3 Fatty Acids (EPA and DHA)
These are found in fish oils—wild-caught salmon, sardine, or anchovy oils tend to be cleaner and more bioavailable than generic “omega blends.” Omega-3s reduce inflammatory prostaglandins and support cellular membrane health. Clinical studies in both humans and dogs have shown that omega-3s can preserve lean body mass, reduce cachexia, and enhance survival when used with chemotherapy.
How much is enough? Effective doses are higher than typical “joint support” formulations—often in the range of 50–70 mg/kg of EPA/DHA combined. But high doses must be balanced against the risk of bleeding or gastrointestinal upset, so veterinary guidance is a must.
Curcumin (from Turmeric)
This golden spice is more than a buzzword. Curcumin has demonstrated anti-inflammatory, antioxidant, and even direct anti-cancer activity in lab studies. The catch? It’s poorly absorbed in the gut unless formulated with lipids or piperine (black pepper extract). So a turmeric powder sprinkled on kibble won’t cut it—you need a bioavailable form.
But here’s the nuance: curcumin can interact with certain chemotherapy drugs, and in high doses may stress the liver. So again, coordination with your care team is key.
Antioxidants
Oxidative stress plays a major role in cancer development, progression, and treatment toxicity. Antioxidants aim to protect healthy cells from damage and help the body recover.
Vitamins C and E
Vitamin C has a complicated reputation—it’s a powerful antioxidant, but at very high doses (especially intravenously), it may act as a pro-oxidant and damage cancer cells. Oral supplementation in dogs is generally safe but should be dosed conservatively. Vitamin E, meanwhile, supports cellular integrity but must be balanced with other fat-soluble nutrients to avoid overdosing.
Coenzyme Q10 (CoQ10)
This compound supports mitochondrial function and energy production. It’s especially useful for dogs who are fatigued or undergoing chemotherapy. Think of CoQ10 as a gentle cellular booster—not a frontline cancer treatment, but a supportive ally in keeping energy levels stable.
Digestive Health
Gut health is foundational. The gut isn’t just where food is digested—it’s a critical immune organ, a hormone hub, and a gatekeeper between the external world and the bloodstream. Cancer (and its treatments) can wreak havoc on the digestive tract.
Probiotics
These are beneficial bacteria that help maintain gut flora balance. Cancer therapies, especially antibiotics and steroids, can wipe out good bacteria. Supplementing with canine-specific probiotics (not just a human capsule or yogurt) can reduce diarrhea, enhance nutrient absorption, and even modulate immune function.
Prebiotics
These are fermentable fibers that feed good bacteria. Think of them as fertilizer for the microbiome. Common sources include inulin and fructooligosaccharides (FOS). They’re often included in comprehensive gut support blends.
Digestive Enzymes
When cancer damages the pancreas or small intestine, nutrient absorption suffers. Enzyme supplements can help break down proteins, fats, and carbs more efficiently—critical for dogs who are losing weight or experiencing malabsorption.
Liver Support
The liver is your dog’s detox powerhouse. It processes medications, metabolizes waste, and clears byproducts of cell turnover—including from dying tumor cells. Keeping it healthy is non-negotiable.
Milk Thistle (Silymarin)
One of the most well-studied liver protectants, milk thistle has antioxidant and anti-inflammatory properties. It’s often used to help detoxify the liver after chemotherapy. Safe in most dogs, but dosing should be adjusted based on weight and liver status.
SAMe (S-adenosylmethionine)
This compound supports liver cell regeneration and methylation. It’s often paired with milk thistle for synergistic effect. Bonus: it may also improve mood and cognitive function in aging dogs.
Anxiety and Pain Modulation
Pain, fear, and anxiety don’t just sap joy—they weaken the body. If your dog is tense, restless, or withdrawn, it’s not just sad—it’s counterproductive to healing.
CBD Oil (Cannabidiol)
CBD is popular, and for good reason. It may help with pain management, anxiety, appetite stimulation, and even inflammation. But the market is flooded with inconsistent products. Look for third-party tested, full-spectrum CBD products designed specifically for dogs.
Is it psychoactive? No—CBD isn’t THC. Your dog won’t get high. But it can cause sedation, changes in appetite, or liver enzyme shifts. Start low, go slow, and loop your vet in.
Herbal Sedatives (Chamomile, Valerian Root, L-Theanine)
These can help ease agitation and promote restful sleep. Most are safe when used at appropriate doses but may interact with other sedatives or seizure meds. They’re best viewed as short-term tools, not daily dependencies.
Up next: we’ll look at how to evaluate and choose supplements, how to dose them, and how to spot signs that they’re helping—or hurting. Because even the best supplement only works if it’s matched correctly to your dog, their diagnosis, and their full treatment picture.
Selecting Quality Supplements — What to Look For and What to Avoid
By now, you’re probably thinking: Okay, I get the categories and potential benefits, but how do I actually choose the right supplements? This is where many well-meaning pet owners get stuck—or worse, get taken for a ride.
Not sure when supportive care turns into palliative care? When to Euthanize a Dog with Cancer is a tough but honest read.
The pet supplement market is a wild west. It’s huge, it’s booming, and it’s lightly regulated compared to pharmaceuticals. That means products vary wildly in quality, potency, and purity. Some supplements labeled as “natural” or “organic” barely contain enough active ingredients to make a difference. Others might be contaminated or even dangerous.
So how do you cut through the noise and pick supplements that truly serve your dog’s health?
Reading Labels: Know What You’re Getting
First, let’s talk labels—the first line of defense.
Does the label list active ingredients clearly and with amounts?
If you see vague terms like “proprietary blend” or “herbal extract” without specific concentrations, be wary. You want to know exactly what’s in there and how much. For example, if a supplement claims to contain turmeric, does it specify how many milligrams of curcumin? Curcumin is the active compound responsible for turmeric’s anti-inflammatory properties, so the amount matters.
Are there unnecessary fillers or additives?
Some supplements include artificial colors, flavors, or preservatives. These aren’t inherently toxic but can cause allergies or sensitivities in sensitive dogs. Look for minimal ingredient lists with recognizable, wholesome components.
Is the supplement formulated specifically for dogs?
Human supplements may contain ingredients safe for people but harmful to dogs. Never assume a human product is safe for your pet without veterinary approval.
Brand Reputation and Transparency
Just like you wouldn’t trust a mechanic who won’t show you their tools, you shouldn’t trust a supplement company that hides its sourcing and testing practices.
- Third-party testing: Look for brands that have their products independently tested by organizations like USP (United States Pharmacopeia), NSF International, or ConsumerLab. This testing confirms potency and absence of contaminants like heavy metals or microbes.
- Good Manufacturing Practices (GMP): Certified manufacturers follow strict protocols to ensure consistency and safety.
- Clear return/refund policies: If a company believes in its product, it will stand behind it.
Dosage and Administration — More Isn’t Always Better
A common misconception is that if a little is good, a lot must be better. This couldn’t be further from the truth with supplements.
How do you know what dose is right?
Dosages often depend on your dog’s weight, cancer type, stage of disease, and whether they’re receiving other treatments. For instance, omega-3 fatty acids are beneficial, but too much can thin the blood and increase bleeding risk, especially if your dog is on certain medications.
Should supplements be given all at once or spaced out?
Some nutrients compete for absorption or may irritate the stomach if given on an empty stomach. Others absorb better with food or fat. Your vet can help design a schedule that maximizes benefits and minimizes side effects.
Signs That a Supplement Is Working—or Not
How do you know if what you’re giving is making a difference? This is critical because it helps avoid wasting money and potentially causing harm.
Positive signs might include:
- Improved appetite and weight stabilization
- Increased energy and activity levels
- Reduced inflammation or pain (sometimes visible as less limping or more playfulness)
- Better digestion and stool quality
- Improved mood and reduced anxiety
Warning signs to watch for:
- New or worsening gastrointestinal upset (vomiting, diarrhea)
- Allergic reactions (itching, swelling, hives)
- Changes in behavior like lethargy or agitation
- Any unexpected bleeding or bruising
- Worsening lab values on veterinary bloodwork
If you see warning signs, stop the supplement and consult your vet immediately.
A Word on Cost
High-quality supplements often cost more. That’s because quality sourcing, third-party testing, and proper manufacturing aren’t cheap. But spending more upfront can save you money—and heartbreak—down the road by avoiding ineffective or unsafe products.
Remember: investing in quality is investing in your dog’s well-being.
The Bottom Line: Be an Informed, Critical Consumer
The most important factor in supplement success isn’t the product itself—it’s you. Your vigilance, your willingness to ask tough questions, your commitment to ongoing monitoring and collaboration with your veterinary team.
Supplements are a tool—a powerful one when used well, but potentially harmful when used blindly.
In the next section, we’ll talk about how to monitor your dog’s response, adjust supplement use over time, and maintain open communication with your vet. Because supplements don’t work in isolation—they’re part of a dynamic process that evolves alongside your dog’s health journey.
Monitoring and Adjusting Supplement Use — Staying Responsive to Your Dog’s Needs
Now that you’ve selected high-quality supplements and begun a regimen, you may find yourself wondering: How will I know if this is actually helping my dog? Or: When is the right time to adjust a dose—or stop altogether if things seem stable? These aren’t just practical questions; they point to a deeper truth about supplements in cancer care: this is not a set-it-and-forget-it situation.
Your dog’s condition is fluid. Their cancer type, their response to treatment, their appetite and energy—all of these things can shift week by week. That means your supplement plan needs to stay flexible, too. What supports healing one month might need adjustment the next. What seemed promising early on could start showing diminishing returns—or even cause problems—down the line.
The key is to stay engaged, observant, and ready to pivot when your dog’s body says, “Something’s changing.”
What Signs Should You Watch For?
Your dog may not be able to speak, but their body is communicating constantly. Sometimes the signs are dramatic; more often, they’re subtle. Being tuned into these signals helps you make informed decisions about whether to maintain, adjust, or discontinue supplements.
Signs of improvement might include:
- Steadier appetite and maintained weight: When your dog is eating consistently and holding or even gaining weight, it’s a strong sign that nutritional and supplement support is working.
- Increased energy and engagement: Cancer and its treatments can sap vitality. If your dog seems more playful, alert, or eager for walks again, you’re likely on the right path.
- Better digestion: Well-formed stools, fewer episodes of vomiting or diarrhea, and reduced gas or bloating all suggest digestive and immune supplements may be doing their job.
- Improved mood and reduced anxiety: If your dog is less restless, sleeping more peacefully, or handling separation better—especially with calming supplements on board—that’s worth noting.
- Reduced signs of inflammation or illness: You may not always see this clearly without bloodwork, but outward signs—like less limping, reduced swelling, or fewer skin flares—can point to internal progress.
Signs that something’s off:
- New or worsening digestive upset: If vomiting, diarrhea, or sudden appetite loss occurs after introducing a supplement, consider it a red flag.
- Behavioral changes: Agitation, lethargy, or signs of discomfort might indicate toxicity, drug interactions, or simply that a supplement is not agreeing with your dog.
- Allergic reactions: Any swelling, hives, intense itching, or difficulty breathing should be treated as a medical emergency. These signs are rare, but serious.
- Unexplained bleeding or bruising: This could signal excessive blood thinning, especially if omega-3s or certain herbs are being used in high doses.
- Lab abnormalities: Routine blood tests can reveal changes in liver enzymes, kidney function, or blood cell counts. A shift here may require stopping or adjusting a supplement—even if outwardly, your dog seems fine.
When and How Should You Adjust a Supplement Protocol?
Fine-tuning a supplement routine isn’t just for experts—it’s something you can do effectively with a little structure and support.
Start with the golden rule: Start low, go slow.
Whenever you begin a new supplement, use the lowest effective dose first and observe your dog closely for 1–2 weeks. This window gives you time to catch any subtle negative reactions before they snowball.
Keep a daily log or supplement journal.
Note what you gave, when, and in what dose. Track your dog’s behavior, appetite, stool quality, mood, and energy levels. It might seem tedious at first, but this kind of recordkeeping becomes invaluable if you ever need to pinpoint a change or share detailed insights with your vet.
Schedule regular veterinary check-ins.
Especially during cancer treatment, lab work every 4–6 weeks is a smart idea. It allows you to track organ function and flag changes early. If your dog is taking liver-support supplements like milk thistle or SAMe, liver enzyme monitoring becomes particularly important.
Be patient, but stay alert.
Some supplements—like CBD or turmeric—can have noticeable effects within days or weeks. Others, like immune modulators or antioxidants, may take longer to show measurable results. That said, if you spot troubling signs, don’t hesitate. Pause the supplement and check in with your vet immediately.
Lastly, be mindful of combinations.
It’s easy to fall into the “stacking” trap—adding immune boosters, joint support, digestive enzymes, and calming agents all at once. But remember: more isn’t always better. Some compounds interact, and others simply overload your dog’s system. If you’re using multiple supplements, introduce them one at a time, with space in between. That way, if something causes a problem, you’ll know where to look.
Should Supplements Be Used Indefinitely?
This is a nuanced issue—and the answer depends entirely on context.
For some dogs, supplements are a short-term tool to support recovery after surgery or to counteract side effects from chemotherapy. For others, especially those in palliative care, supplements become part of a long-term wellness strategy, helping maintain comfort and function even as the disease progresses.
And yes, there are cases when it makes sense to pause or stop supplementation. This might be due to side effects, lack of benefit, or changes in your goals of care. For example, if your dog’s cancer enters an advanced, non-treatable stage, the focus may shift toward comfort-only measures, and supplements that once supported aggressive care may no longer serve a purpose.
The key here is to remain flexible and communicative. Your supplement protocol should evolve as your dog’s needs evolve. It’s not failure to stop something; it’s wisdom.
Collaborating with Your Veterinarian
If there’s one thing that amplifies the benefit of any supplement, it’s collaboration. Your veterinarian is not just there to diagnose and prescribe—they’re your partner in refining your dog’s care.
Here’s how to make that partnership count:
- Bring your research and your curiosity. Don’t worry about “annoying” your vet with questions. Show them you’ve done your homework and explain your intentions.
- Be transparent about what you’re giving. Include specific product names, doses, and timing. Don’t assume they’ll approve or disapprove—invite them into the conversation.
- Report changes early. If you notice improvements, great—share them. But if anything seems off, loop your vet in quickly.
- Ask about lab monitoring. Some vets may not automatically check liver or kidney function during supplement use. Ask if periodic bloodwork is appropriate based on your dog’s regimen.
- Stay open to expert feedback. Your vet may suggest halting a supplement, reducing a dose, or switching to a different form. Remember: this isn’t criticism—it’s refinement.
Being proactive, observant, and collaborative isn’t just about managing supplements—it’s about honoring the complexity of your dog’s body and the seriousness of the disease you’re facing together. You don’t have to be a veterinary professional to think like one. By watching closely, adjusting carefully, and partnering intentionally, you can give your dog the best support possible—not just through what you give, but how you give it.
Frequently Asked Questions (FAQ)
You’ve covered a lot of ground so far—understanding canine cancer, the role of nutrition, the types of supplements, how to choose and monitor them, and real-life stories. But even with all that, some questions naturally linger. Maybe you’re thinking, “Is this really safe?” or “How long before I see results?” or even “Can supplements interfere with chemotherapy?”
1. Can supplements cure my dog’s cancer?
No. Supplements are not cures. They support your dog’s body and can improve quality of life, possibly even extend survival time when used alongside conventional treatments. But cancer is complex and requires comprehensive care.
2. Are there risks associated with supplement use?
Yes. Natural doesn’t mean risk-free. Supplements can cause side effects, interact with medications, or worsen certain conditions. That’s why veterinary guidance is essential before starting any new supplement.
3. How do I know which supplements are right for my dog?
It depends on your dog’s specific cancer type, treatment plan, and overall health. Consult with your vet or a veterinary nutritionist who can tailor a plan based on your dog’s needs.
4. Can I use human supplements for my dog?
Generally, no. Dogs metabolize substances differently, and doses safe for humans can be toxic to dogs. Always use products formulated specifically for pets, and check with your vet.
5. How long does it take to see results from supplements?
It varies. Some benefits like improved appetite or mood can appear in days or weeks. Others, such as immune support or anti-inflammatory effects, may take several weeks to months. Patience and consistent monitoring are key.
6. Should supplements be used alongside conventional cancer treatments?
Yes, but with careful coordination. Supplements can support chemo or radiation by reducing side effects and boosting health. However, some supplements may interfere with treatment efficacy, so always discuss with your oncologist.
Closing Thoughts
You’ve taken a deep dive into a challenging and often overwhelming topic: supplements for dogs with cancer. Along the way, we’ve unpacked what cancer really means for your dog, why nutrition matters so much, how different supplements can support various aspects of health, and the importance of thoughtful selection and monitoring. We’ve even looked at real-world stories and answered tough questions.
So where does all this leave you?
First: You are your dog’s greatest advocate. Nobody knows your dog better than you do. That’s a powerful position. Supplements are tools—complex, nuanced, sometimes confusing—but with the right information, they become extensions of your care and love.
You might be asking yourself: “Am I doing enough? Could I do more?” The honest answer is: you’re doing everything you can with what you know, and that’s exactly what matters. What this guide aims to give you is not just facts but confidence—to ask the right questions, to recognize good advice, and to make decisions informed by both science and compassion.
Cancer in dogs is hard. It’s unpredictable and emotionally wrenching. But it’s also a journey where every day matters—where quality of life can be nurtured and hope sustained, even in the face of uncertainty.
Supplements won’t cure cancer. They won’t replace surgery, chemotherapy, or radiation. But when chosen wisely and used carefully, they can support your dog’s body in ways that ease suffering, bolster resilience, and sometimes extend precious time together.
Remember, the best outcomes come from partnership—between you, your dog, your veterinarian, and when possible, specialists like veterinary nutritionists and oncologists who understand the integrative approach. Share your observations openly. Celebrate the small wins. Adjust when needed.
Lastly, never underestimate the power of presence—your love, your touch, your voice. Those are supplements no pill can replicate.
Thank you for taking this journey with care, intelligence, and heart. Your dog is lucky to have you.
If you revisit this guide, share it, or keep it close, may it always remind you that knowledge is strength, and strength is hope.