Can Root Canals Cause Cancer? Myths vs. Medical Facts
- Part 1: Understanding Root Canal Treatment
- Part 2: The Origin of the Cancer Myth
- Part 3: Scientific Evidence Against the Myth
- Part 4: The Role of Misinformation
- Part 5: The Real Risk? Avoiding the Root Canal
- Part 6: What the Experts—and the Patients—Know
- Part 7: Root Canal vs. Extraction — Weighing the Real Trade-offs
- Part 8: Prevention Is Power — Keeping Root Canals Off the Table
- Part 9: Final Thoughts — Reclaiming Trust in the Age of Medical Noise
Foreword
Let’s talk about something that pops up every few years, spreads like wildfire online, and leaves a trail of anxious patients in dental chairs worldwide: the claim that root canals can cause cancer. If you’re here, chances are you’ve heard a friend mention it, stumbled upon a viral video, or seen a documentary that left you second-guessing a treatment your dentist recommended. You’re not alone—and you’re right to be curious. In fact, the very act of questioning what you’ve been told is a mark of critical thinking. That’s what we’ll honor and build upon in this article.
Because the truth is, this isn’t just about teeth. It’s about trust—trust in medical science, in your healthcare providers, and maybe even in your own body. And when a claim arises that a common dental procedure—performed more than 15 million times a year in the U.S. alone—might be hiding a dark secret, it deserves a proper examination. Not an echo chamber of fear. Not a glossed-over reassurance. But a deep, honest, evidence-informed investigation.
We’re going to look at where this myth came from, why it persists, and what science has to say about it today. You’ll meet the researchers, the skeptics, and the dentists caught in the crossfire of public mistrust. Most importantly, you’ll leave knowing whether root canals are something to worry about—or just another medical myth that thrives in the age of clickbait.
So let’s begin, not by brushing anything under the rug, but by asking the question straight out: what exactly is a root canal?
Understanding Root Canal Treatment
We’ve all heard of them. We’ve all dreaded them. But few people outside of dentistry actually know what a root canal is. So let’s strip away the jargon and get down to the core—pun absolutely intended.
What Is a Root Canal?
At its heart, a root canal is a medical procedure designed to save your natural tooth. That’s right—save, not destroy. It’s not some dental equivalent of sealing radioactive waste in your jaw, as some fear-driven corners of the internet might suggest.
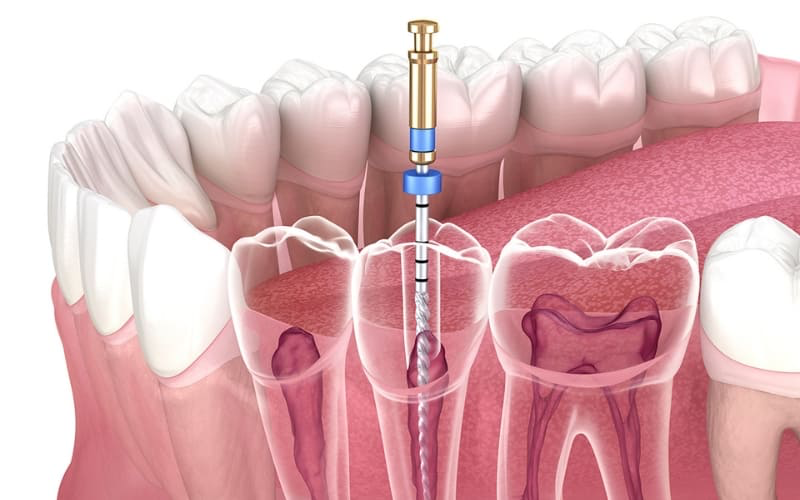
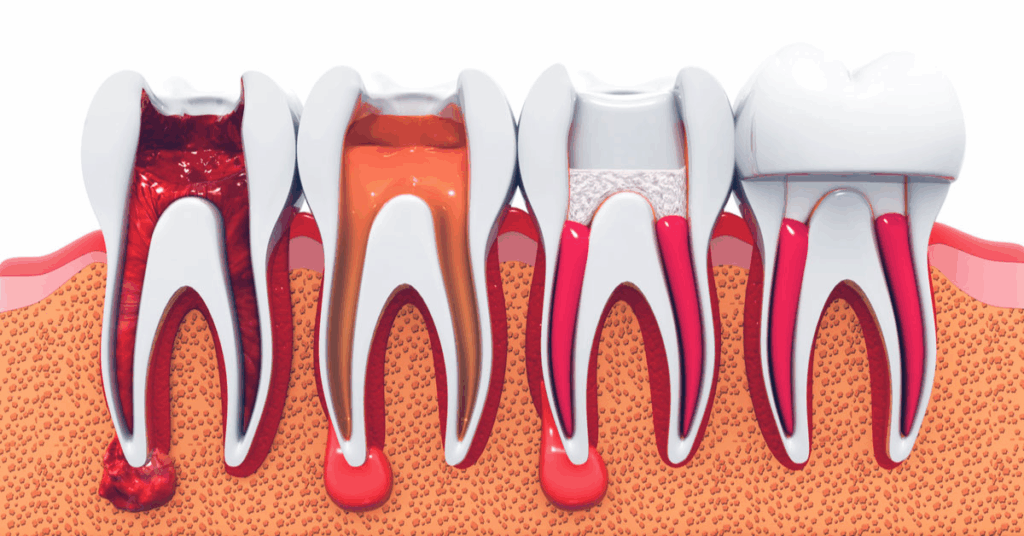
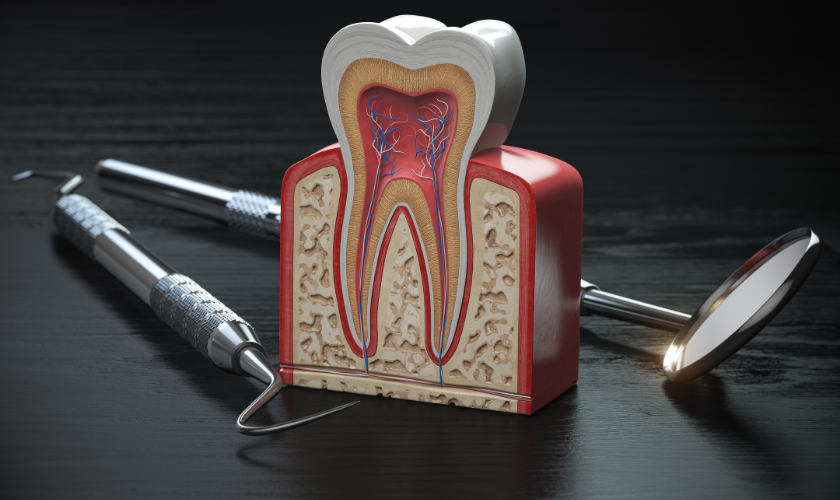
Inside each tooth lies a soft core of tissue known as the pulp. This pulp contains nerves, blood vessels, and connective tissue that help the tooth grow during development. But once a tooth is fully grown, it can survive just fine without the pulp. So if that pulp becomes infected—due to a deep cavity, a crack, or trauma—it needs to be removed. Why? Because infection doesn’t just sit quietly. Left untreated, it can spread to the surrounding bone, your bloodstream, and even cause systemic inflammation.
That’s where the root canal procedure comes in.
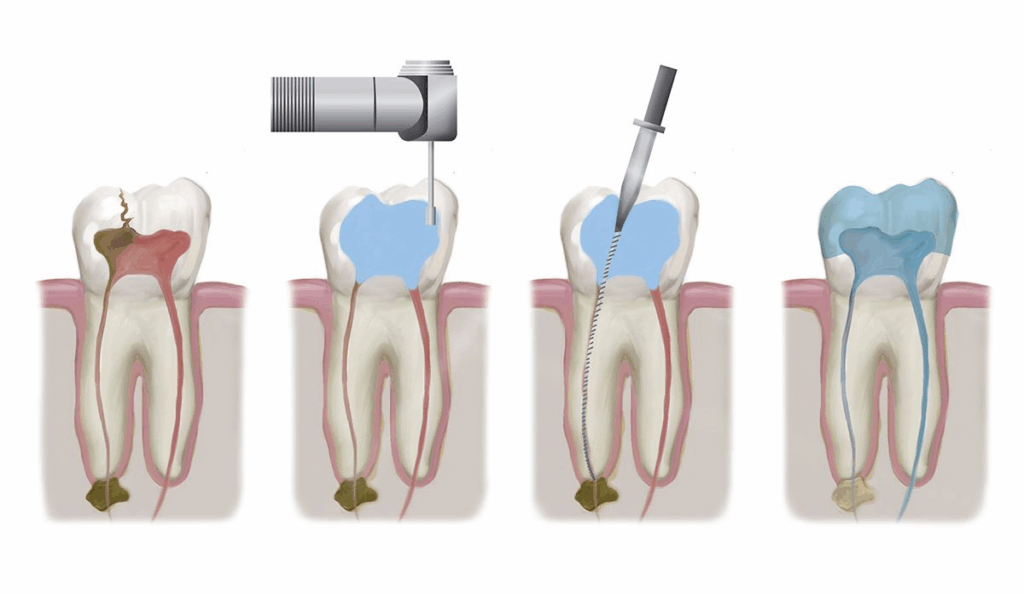
During a root canal, your dentist or endodontist (a root canal specialist) removes the infected or dead pulp, carefully cleans and shapes the inside of the root canals, and fills the space with a biocompatible material. Finally, the tooth is sealed and usually topped with a crown to restore its full function. That’s it. No black magic. No trapped toxins. Just targeted cleaning and restoration.
Why Are Root Canals Even Necessary?
Let’s address a natural question: Why not just pull the tooth? Wouldn’t that be easier? In some cases, yes—but often, no.
Preserving a natural tooth is almost always preferable. Extracting a tooth creates a domino effect: neighboring teeth may shift, chewing becomes less efficient, and jawbone atrophy can occur over time. Not to mention the emotional and cosmetic impact of losing a visible tooth.
Root canals allow you to keep your natural tooth in place, functioning as nature intended. And thanks to advances in technology, the procedure is now about as comfortable as getting a filling. Local anesthesia, rotary tools, digital imaging—it’s not your grandfather’s root canal anymore.
Are Root Canals Safe?
Yes. Categorically and repeatedly, yes.
But before we go too far down that road, we’ll devote a full section to answering that question with data. Still, it’s worth acknowledging that fear doesn’t usually spring from a vacuum. So where did this suspicion come from in the first place? Who lit the match that sparked a century-long debate? And why do conspiracy theories around dental procedures have such staying power?
In the next section, we’ll dive into the origin story of this myth—one that involves a well-meaning but mistaken researcher, outdated science, and a modern internet that never forgets.
Spoiler: you’re about to meet Dr. Weston A. Price. Buckle up.
The Origin of the Cancer Myth
Let’s rewind the clock a bit—to a time when dentistry was more guesswork than science and sterilization was still a luxury, not a standard. That’s the early 20th century. It was in this uneasy context that a man named Dr. Weston A. Price rose to prominence.
Now, if you’ve ever gone down a rabbit hole about the dangers of root canals, his name might sound familiar. To some, he’s a visionary. To others, a cautionary tale. But to truly understand how the root canal–cancer myth came to be, you have to understand his story.
Dr. Price was a Canadian-born dentist and researcher whose ideas would later become lightning rods in debates over nutrition, dental health, and yes, systemic disease. His most influential work came from his “focal infection theory”—the belief that infections in one part of the body, particularly the mouth, could lead to chronic diseases elsewhere. This wasn’t pulled out of thin air. At the time, germ theory was still being explored, and medical science was actively trying to connect dots between visible infections and invisible systemic illnesses.
Price’s theory zeroed in on root canal-treated teeth as a particularly dangerous culprit. He conducted experiments—decidedly unrigorous by modern standards—in which he would extract root canal-treated teeth from sick patients, implant them under the skin of rabbits, and then observe the rabbits for signs of illness. Unsurprisingly, the rabbits often got sick. But here’s the rub: these were already severely ill human teeth, implanted into immune-defenseless animals in a pre-antibiotic era. That’s not science; that’s anecdote with lab coats.
And yet, his findings were widely accepted for a time. Remember: this was a period when even appendicitis was treated with dental extractions because people feared hidden “oral sepsis.” The bar for medical evidence was low, and Price’s theories filled a vacuum of understanding. It took decades—and many better-designed studies—to dismantle his conclusions.
So why does his work still matter? Because myths, once seeded, don’t disappear just because science catches up. They linger. They evolve. They adapt to modern anxieties.
The focal infection theory was officially discredited by the 1950s and ’60s, thanks to mounting evidence from microbiology, immunology, and clinical dentistry. Researchers began to show that root canal-treated teeth, when properly sealed, did not harbor dangerous levels of bacteria. They did not leach toxins. And they did not contribute to chronic illness. But as the scientific consensus moved on, public perception lagged behind.
Then came the internet.
In 2019, a documentary titled Root Cause was released on Netflix. It echoed Price’s century-old claims, only this time wrapped in high-production value and health-and-wellness buzzwords. The film alleged that root canals trap toxins, cause immune dysfunction, and are linked to everything from heart disease to—you guessed it—cancer. It cited selectively, relied heavily on anecdotal accounts, and failed to provide a shred of high-quality peer-reviewed evidence. Dental and medical communities responded swiftly. The American Dental Association, the American Association of Endodontists, and others condemned the film, which was eventually pulled from Netflix. But the damage was done.
Even now, if you search “root canals cancer,” you’ll find blog posts, YouTube videos, and influencer testimonials citing this film or Price’s century-old theories as fact. And here’s the difficult part: some of the fears feel intuitively plausible. If there’s infection deep in your body—even in a tooth—shouldn’t that be cause for concern? If you “seal” something bad inside a tooth, doesn’t that create a ticking time bomb?
It’s a reasonable line of questioning. But it’s also exactly where science steps in—not to dismiss those concerns, but to test them, rigorously and repeatedly.
And that’s what happened. Over the past several decades, study after study has asked: Do root canals contribute to chronic disease? And, more specifically, Is there any evidence linking root canals to cancer?
The answer—no matter how many ways you slice it—is no.
But don’t take that on faith. In the next section, we’ll pull back the curtain on the science: the large-scale studies, the professional statements, and the cold hard data that settle the question far better than anecdote ever could.
Because if there were even a sliver of reliable evidence connecting root canals to cancer, you’d want to know, wouldn’t you? Good. So would we. And we’ve looked. Hard. Let’s get into what we found.
Scientific Evidence Against the Myth
So, we’ve looked at where the cancer claim came from—a mixture of outdated science, misapplied logic, and modern-day fear amplification. But what does current science actually say? Is it just a matter of opinion—dentists saying “trust us”—versus skeptics saying “prove it”? Or do we have real, clinical, peer-reviewed data to lean on?
We do. And it’s robust.
Let’s start with a simple premise: if root canals did increase cancer risk, we would expect to see this play out across population data. We’d see patterns. Trends. Clusters. After all, millions of people undergo root canal treatment every year. If that procedure were even marginally increasing the risk of cancer, epidemiologists would have picked up on it. And if they had, it would have made headlines in every major medical journal and newspaper. But that hasn’t happened—not even close.

One of the most cited studies comes from a team at the University of Michigan School of Dentistry. In a 2013 paper published in Cancer Epidemiology, Biomarkers & Prevention, researchers followed over 460 participants and found something remarkable: people who had undergone one or more root canals had a slightly decreased risk of head and neck cancer compared to those who hadn’t. Decreased. Let that land.
That finding may sound counterintuitive at first—why would treating a tooth infection lower cancer risk? The answer is likely less about the root canal itself and more about the kind of person who receives one. People who seek timely dental care tend to take better care of their health overall. They’re more likely to address infections promptly, maintain good hygiene, and follow up with preventive medical care. In short, they’re proactive. And that proactivity, across a lifespan, can influence health outcomes in profound ways.
Still, one study isn’t enough to close the book. Fortunately, we have more.
Other large-scale cohort studies, including data pooled from cancer registries and dental records, have shown no statistically significant correlation between root canal therapy and the development of systemic diseases—including cancer. The American Association of Endodontists (AAE) has compiled decades of such research, reinforcing a consistent conclusion: root canal-treated teeth do not contribute to cancer, autoimmune disease, or other systemic conditions.
Why, then, do claims to the contrary persist?
Because once a narrative takes hold—especially one that connects something as terrifying as cancer to a procedure most people already dread—it sticks. And because cancer, by nature, is elusive. It’s multifactorial, often slow-developing, and frustratingly non-linear. This opens the door to what researchers call causation confusion. If someone gets a root canal and then, years later, is diagnosed with cancer, the temptation to connect the two dots is powerful—even if there’s no scientific reason to.
But that’s correlation, not causation. And science has tools to parse the difference.
Let’s pause here and consider a different but related example: vaccines and autism. One discredited study in the 1990s sparked a global controversy that still hasn’t died down, despite a mountain of evidence disproving the link. The root canal myth follows a similar arc. A single flawed theory, amplified by selective storytelling and the internet’s echo chamber, becomes a cultural virus—resistant to facts but not immune to them.
Fortunately, when health organizations respond, they don’t just issue vague reassurances. They bring receipts.
The American Dental Association, the American Cancer Society, the Centers for Disease Control and Prevention, and the World Health Organization have all stated—either directly or through their educational content—that root canal therapy is safe. No link to cancer. No lingering toxins. No mystery infections hiding in your mouth waiting to strike. What we’re dealing with here isn’t a medical risk. It’s a myth that refuses to go quietly.
That’s not to say root canals are risk-free in an absolute sense. Like any medical procedure, they can fail. Teeth can re-infect. Improper technique or poor hygiene can lead to complications. But those risks are localized and manageable—not the stuff of systemic disease or long-term bodily harm.
The notion that a tooth treated, disinfected, and sealed with today’s technology could harbor “trapped toxins” that somehow evade your immune system for years before triggering cancer? That’s not just unlikely—it’s biologically implausible. Your body’s immune system is not a passive observer. It actively monitors and responds to threats every second of your life. If a root canal-treated tooth were leaking harmful substances, we wouldn’t need Netflix documentaries to sound the alarm. Your own physiology would do that job quite effectively.
So if you’re someone who cares about health, who values science, and who doesn’t want to fall prey to fear-based medicine, the evidence is clear. Root canals don’t cause cancer. They treat infection. They preserve teeth. They improve quality of life. And they do so with a safety record stretching across decades.
Still, we understand: myths die hard, especially when they get wrapped in half-truths and emotional storytelling. That’s why in the next section, we’ll examine just how powerful misinformation can be—and why even the best science sometimes struggles to compete with a good scare story.
The Role of Misinformation
By now, you’ve seen the data. You’ve seen the scientific consensus. So it begs a difficult question: Why is this myth still alive? Why, after more than half a century of research debunking the root canal–cancer connection, are we still talking about it?
The answer lies not in the science, but in the psychology—and increasingly, the algorithms.
Misinformation spreads not because it’s true, but because it’s compelling. It’s sticky. It hijacks your attention by triggering emotions—fear, outrage, suspicion—all of which make us more likely to share a story without verifying it. And in the case of health misinformation, there’s an even more potent emotional cocktail at play: anxiety about the unknown, distrust in institutions, and the basic human drive to protect ourselves and our loved ones.
Let’s take a closer look at one of the most powerful vectors of this myth in modern memory: the 2019 documentary Root Cause. Professionally shot, emotionally charged, and filled with anecdotal testimonials, it didn’t need to prove anything scientifically—it just needed to feel right to the viewer. That’s what made it so effective. The central narrative was elegant in its simplicity: “I was sick for years. I didn’t know why. Then I removed my root canal-treated teeth—and I got better.”
It’s an emotionally satisfying arc. Problem, discovery, solution, resolution. What it lacks in medical rigor, it makes up for in storytelling clarity. Unfortunately, real health outcomes don’t work that cleanly. Recovery is rarely linear. Chronic illness is often multifactorial. And most importantly, anecdote is not evidence.
But that distinction gets blurred when you watch someone on screen tearfully describe how their symptoms vanished after dental surgery. You want to believe them. Who wouldn’t?
The issue isn’t whether that person is telling the truth. The issue is that their experience can’t be generalized. We don’t know what other factors were involved, what confounding variables were at play, or whether any improvement was simply the result of the placebo effect, natural recovery, or coincidence. It’s not that these stories should be dismissed out of hand—they should be contextualized. And that’s exactly what these films refuse to do.
Social media takes the problem a step further. Posts that make shocking claims—“Your dentist is hiding this from you!” or “The deadly secret behind root canals!”—perform far better in terms of engagement than posts that say, “Root canals are safe, and here’s a link to a meta-analysis.” One gets clicks. The other gets ignored. So guess which one keeps getting surfaced by the algorithm?
Even worse, platforms like YouTube and TikTok reward creators who generate high watch times and shares. That creates a perverse incentive: don’t be accurate, be outrageous. The more extreme the claim, the more traction it gets.
And once a person starts watching or interacting with content that’s suspicious of conventional medicine, they often get funneled into broader conspiratorial communities: anti-vaxxers, alternative cancer cure advocates, fluoride truthers. Before long, a simple question about a dental procedure turns into full-blown medical skepticism.
That’s not to say all alternative views are invalid. Science is never “finished,” and medical consensus evolves. But the difference between skepticism and cynicism is huge. Skepticism asks questions and considers evidence. Cynicism assumes bad faith and cherry-picks whatever supports its narrative.
There’s also a deeper layer at play: an erosion of trust. Many people genuinely feel that modern healthcare has failed them—rushed appointments, confusing bills, or treatments that didn’t work. That frustration is real. And when someone offers a simple, emotionally resonant explanation for why you’re suffering—“It’s your root canal!”—it can feel more validating than hearing, “Well, chronic fatigue is complex, and we’re still figuring it out.”
Misinformation doesn’t just fill a knowledge gap. It fills an empathy gap.
So how do we counter it?
Not with ridicule. Not with snark. But with clarity, respect, and an unflinching commitment to nuance. We acknowledge that medical systems aren’t perfect—but we also stand up for what is well-understood and evidence-backed. Root canals, when done properly, are safe. Full stop.
We also counter it by empowering patients—giving you tools to spot red flags, to evaluate sources, to understand the difference between correlation and causation. Because if you’ve read this far, chances are you’re not looking for a viral soundbite. You’re looking for clarity. You’re looking for science that respects your intelligence. And you deserve nothing less.
In the next section, we’ll zoom out again—not into theory or myth, but into real-world implications. Because while cancer might be the headline-grabber, there’s another silent threat: what happens when people avoid root canals out of fear? What happens when infections are left untreated, when dental decay goes unchecked? Ironically, the thing we’re afraid of might not be the treatment—but the cost of skipping it. Let’s talk about that.
The Real Risk? Avoiding the Root Canal
Let’s set aside the cancer myth for a moment and entertain a different kind of scenario—one that’s far more common, far more immediate, and ironically, far more dangerous. It doesn’t involve cover-ups or secret toxins. It involves avoidance.

Imagine you’ve got a nagging toothache. It flares up when you drink something hot or cold, maybe keeps you up at night. Your dentist tells you the pulp is infected and recommends a root canal. But you hesitate. You’ve seen that documentary, read that blog post, watched a friend rant on Instagram. So instead of going through with the procedure, you wait. You decide to “see how it goes.”
At first, the pain lessens. That’s not a good sign—it means the nerves inside your tooth are dying. You’re not healing; you’re progressing. The bacteria don’t stop just because you did. They move deeper. Into the root tips. Into the surrounding bone. Eventually, they could breach the bloodstream, especially if you’re immunocompromised. Now you’re looking at systemic inflammation. Maybe even a hospital visit.
This isn’t fear-mongering. It’s anatomy. When oral infections go untreated, the consequences don’t stay neatly within your mouth. Your teeth are connected to a living, vascular system. Infection spreads. That’s biology doing exactly what biology does.
Let’s be honest: it’s understandable why people avoid root canals. They’re often expensive. The reputation (however outdated) is intimidating. And if you’ve been exposed to misinformation, the idea of “sealing in toxins” can sound downright sinister. But here’s the paradox: in trying to avoid a perceived risk, you may be creating a very real one. Dental infections don’t magically resolve. They don’t shrink with turmeric or essential oils. They fester.
The end result? You might find yourself needing an extraction. Not ideal.
Now, to be fair, there are times when extracting a tooth is the right call. But doing it by default—especially because of misinformation—isn’t protecting your health. It’s compromising it. Losing a tooth sets off a cascade: neighboring teeth can drift, your bite can destabilize, bone can begin to atrophy. Even with an implant, which is often the next step after an extraction, you’re still dealing with more cost, more surgery, and more recovery time than you’d face with a root canal and crown.
And let’s not forget the psychological aspect. People underestimate the emotional toll of tooth loss. It affects self-confidence, speech, eating habits. And once one tooth goes, others often follow. A single untreated infection can spiral into a pattern of decline.
So why aren’t more people talking about this risk? Why doesn’t “Avoiding root canals leads to complications” go viral?
Because it’s not sensational. It’s gradual. It doesn’t lend itself to a shocking YouTube thumbnail or a dramatic personal testimonial. It’s just the slow, unglamorous march of neglect catching up to biology.
And yet, this is the narrative we need to emphasize. Not because we’re trying to sell you a procedure, but because your long-term health depends on it. Dental infections are real. Their consequences are measurable. And root canals, when done right, are an elegant solution: clean the infection, preserve the structure, restore function. It’s a triumph of conservative dentistry.
But perhaps most importantly, they’re an act of prevention. Not just of pain, but of escalation. They stop a small issue from becoming a big one.
You might still have doubts. That’s okay. Healthy skepticism is a strength. But make sure that skepticism is directed at the right target. Be skeptical of anyone selling fear without data. Be skeptical of claims that promise perfect health if you just pull all your teeth or avoid “conventional” treatments. Be skeptical of narratives that villainize entire professions without offering credible alternatives.
Because the real risk here isn’t the root canal. It’s letting fear steer your decisions when your body—and the science—are telling you something else entirely.
Next, we’ll hear directly from the people on the front lines: the dentists and endodontists who perform these procedures every day, and the patients who’ve lived through both the fear and the relief. What do they know that the internet doesn’t? Let’s find out.
Root Canal vs. Extraction — Weighing the Real Trade-offs
Let’s be pragmatic. Even if you’re no longer worried that a root canal will stealthily give you cancer, you might still be asking a valid question: If my tooth is this far gone, wouldn’t it be easier to just pull it? Isn’t extraction simpler, faster, and potentially cheaper?
That instinct isn’t wrong. Extraction often is faster. It may even cost less in the short term. But as with most decisions in medicine, the immediate fix isn’t always the best long-term choice. Tooth extraction isn’t the dental equivalent of decluttering your mouth. It comes with a cascade of consequences that are often invisible at first—and expensive later.
Let’s unpack this, not as a scare tactic, but as a sober look at biological reality.
Here’s what happens when a tooth is removed: you don’t just create a gap in your smile; you create a vacuum in your bite mechanics. Teeth are not solitary structures. They’re interdependent, held in place and in function by the pressure and presence of neighboring and opposing teeth. Pull one out, and others begin to shift, tilt, and migrate. Your bite alignment can change. Chewing becomes less efficient. Even jaw posture and speech can be subtly altered. These shifts aren’t dramatic overnight changes—they’re slow, often silent—but once the balance is thrown off, it rarely self-corrects.
That’s when bone loss begins.
The roots of your teeth don’t just anchor chewing function—they stimulate the underlying bone through pressure. When a tooth is removed, that pressure disappears, and your body begins to resorb the now-unused bone. Within a year, you can lose up to 25% of the bone volume in that area. Multiply that by several extractions, and you’re not just looking at cosmetic concerns—you’re facing structural issues that affect your entire lower face.
Now imagine that happening before you’ve even hit middle age. This is why many people who’ve lost several teeth find that dentures don’t fit well after a while. The shape of their jaw is literally changing. The scaffolding is shrinking.
Let’s say you’re proactive and plan to replace the extracted tooth with an implant. Good. But here’s the reality: you’re now signing up for more procedures, more time in the chair, and significantly more expense. A single dental implant (post, crown, and abutment) can run anywhere from $3,000 to $6,000 depending on geography and complexity. And not everyone is a candidate—some people don’t have enough remaining bone to anchor the implant securely and may need bone grafting first, adding more time, money, and surgical intervention.
Compare that to a root canal, which—assuming no major complications—typically costs less and is completed in one or two visits. When followed by a crown, the treated tooth can last decades, functioning and looking just like its neighbors. No jawbone shrinkage. No shifting. No surgical follow-ups.
It’s not that extraction is always wrong. There are scenarios where it makes sense—teeth with vertical root fractures, severe mobility from bone loss, or a history of multiple failed root canals. Sometimes, yes, the best path forward is to remove the problem altogether. But that decision should be made based on structural viability and overall oral health—not on fear of outdated or misrepresented science.
A tooth is not just a piece of calcium. It’s part of a system—biomechanical, aesthetic, and emotional. People often underestimate how strongly they’ll feel the loss of a tooth, especially a visible one. The psychological impact is real. Even if no one else can see the gap, you know it’s there. That awareness changes how you smile, speak, and sometimes even how you eat.
And let’s not forget maintenance. Once a tooth is gone, you’re forever in the business of replacing it—or dealing with the fallout of not doing so. Bridges can stress surrounding teeth. Partials can feel awkward. Implants, while excellent, require surgical skill and diligent hygiene to avoid complications like peri-implantitis. Each of these solutions is useful in the right context, but none of them are as biologically simple and self-sustaining as keeping your natural tooth alive.
That’s what root canals offer: the chance to press pause, clean the slate, and start again with your own tooth. No prosthetics. No removables. Just your tooth, restored.
So when you’re weighing root canal versus extraction, don’t just weigh the pain or the price tag. Weigh the future. Weigh the domino effect of removing a piece from the puzzle. Ask yourself not just what will fix this moment, but what will protect the next ten years of your oral health.
Because treating one tooth wisely is never just about that tooth. It’s about everything that comes with it: the alignment, the integrity, the confidence. In dentistry—as in life—sometimes the harder choice is the one that holds everything else together.
Lastly, it’s worth seeing how oral cancers actually develop, so you have context on risk versus coincidence. That’s broken down clearly in How Oral Cancer Spreads.
Coming up next: the steps you can take to reduce your risk of ever needing a root canal in the first place. Because prevention? That’s where the real magic happens.
Prevention Is Power — Keeping Root Canals Off the Table
So far, we’ve walked through the fears, the facts, and the fallacies. But what if you could sidestep the whole question of root canals entirely? Not because you’re dodging a necessary treatment, but because you’ve made the need for one almost obsolete?
That’s not wishful thinking. That’s preventive dentistry—and it’s far more potent than it gets credit for.
Let’s start with a quiet truth that rarely gets the spotlight: most root canals are avoidable. Not all, of course. Sometimes trauma strikes—a sports injury, a hidden crack, a surprise abscess. Life happens. But the vast majority of root canals stem from one simple, slow-moving cause: untreated decay. Cavities that aren’t caught. Fillings that are delayed. Hygiene that breaks down over time.
And here’s the kicker: decay doesn’t leap from zero to root canal overnight. It progresses. It gives off warning signs. It even throws up a few red flags if you’re paying attention. That’s what makes prevention not just powerful—it’s practical. You can see it coming.
So how do you avoid landing in a dentist’s chair with that dreaded recommendation?
It starts where you probably expect: brushing and flossing. Yes, it sounds elementary. But the boring basics are what protect you. Twice a day with fluoride toothpaste, at least once a day with floss, and—this part is crucial—with techniquethat actually disrupts plaque. Brushing for 20 seconds in a hurry isn’t the same as two focused minutes with good coverage. Flossing just your front teeth isn’t enough. If you’re not cleaning between molars, you’re skipping the most cavity-prone surfaces in your entire mouth.
But daily hygiene, while essential, isn’t enough by itself. The real heavy lifter in long-term dental health? Consistent, preventive checkups.
That’s where the real wins happen. Early detection. Tiny cavities that can be stopped in their tracks with small, inexpensive fillings. Weak spots that can be remineralized before they become irreversible decay. Gum inflammation that can be reversed before it leads to bone loss. These appointments aren’t just about scraping tartar and handing out toothbrushes—they’re about intercepting future problems while they’re still small, manageable, and painless.
But there’s another layer here, and it’s not just technical. It’s strategic.
Ask any dentist, and they’ll tell you that prevention is as much about behavior as it is about brushing. Diet plays a massive role. Sugary snacks, acidic beverages, frequent grazing—these feed the bacteria that cause cavities and wear down enamel. And it’s not just what you eat—it’s how often. Constant sipping of soda or even fruit juice can bathe your teeth in acid all day long, keeping the pH low and the risk high.
Want to make a tangible change? Cut out frequent between-meal sipping. Switch to water. Be mindful of “health” foods that are stealthily high in sugar or acid—like dried fruit, flavored yogurts, and sports drinks. None of this is about perfection. It’s about understanding your risk profile and shifting habits that tilt the odds in your favor.
And for those with deeper vulnerabilities—whether due to genetics, medication side effects, or chronic conditions like diabetes—there are extra tools in the toolkit. Prescription-strength fluoride toothpaste. Sealants. Xylitol. Saliva stimulants. Custom trays for fluoride application. None of these are high-profile solutions, but they’re backed by evidence and can dramatically reduce the chance of ever needing invasive treatment.
Perhaps most empowering of all is the shift in mindset. When you move from reactive to preventive care, dentistry stops being a series of expensive surprises and becomes a structured, predictable routine. That’s good for your health—and your wallet.
Because let’s be real: no one wakes up hoping for a root canal. Even knowing it’s safe, even knowing it won’t cause cancer, it’s still time, money, and recovery. But what’s even better than a successful procedure is not needing one at all. Prevention is freedom. It’s control. It’s the quiet confidence of walking into a dental visit knowing you’ve done your part—and knowing your dentist will likely find nothing to fix.
In the next section, we’ll take a breath and zoom out one last time. All the fear, the misinformation, the procedures, the evidence—it all comes down to a simple but deeply personal question: what kind of health story are you writing for yourself? And what role does trust—real, informed trust—play in that journey?
We’ll wrap this up with some closing thoughts that put everything in perspective.
Can a root canal really cause cancer?
No. There is no credible scientific evidence linking root canal treatments to cancer. Decades of research and epidemiological data show no increased cancer risk in people who have had root canals.
Where did the root canal–cancer myth come from?
The myth traces back to early 20th-century research by Dr. Weston A. Price, whose flawed experiments were later discredited. The idea resurfaced through modern media but remains unsupported by science.
Are there any health risks from root canal-treated teeth?
Complications can happen if a root canal fails (e.g., due to missed anatomy or poor sealing), but these are localized dental issues—not systemic or cancer-causing conditions.
Is tooth extraction safer than a root canal?
Not necessarily. Extraction may seem simpler, but it can lead to bone loss, shifting teeth, and expensive replacements. When possible, preserving the natural tooth is the better long-term choice.
What are signs I might need a root canal?
Persistent tooth pain, sensitivity to heat or cold, swelling, or a pimple-like bump on the gum can indicate infection or damage to the pulp—conditions a root canal is designed to treat.
How can I reduce the chance of ever needing a root canal?
Maintain excellent oral hygiene, limit sugary or acidic foods, and visit your dentist regularly for early detection and intervention. Prevention is the best treatment.
Final Thoughts: Trust, Clarity, and Moving Forward
At its core, this wasn’t just a story about root canals. It was about trust—how we build it, how we lose it, and how we reclaim it in a world crowded with contradiction.
Yes, medical science evolves. Yes, it’s imperfect. But root canal therapy is no mystery. It’s studied, standardized, and safe. The idea that it causes cancer simply doesn’t hold up—not in clinical outcomes, not in epidemiological data, not in basic biology.
You’re right to ask questions. But let those questions lead you toward evidence, not fear. In the end, this isn’t about a tooth. It’s about your right to understand what’s real and what’s noise—and to choose your care with clarity.