How Insulin Resistance Is Linked to Triple-Negative Breast Cancer
- Foreword
- Part 1: What Is Insulin Resistance?
- Part 2: What Is Triple-Negative Breast Cancer (TNBC)?
- Part 3: The Link Between Insulin Resistance and Triple-Negative Breast Cancer
- Part 4: How Insulin Resistance Affects TNBC Tumor Growth
- Part 5: Implications for Treatment
- Part 6: Prognosis and Outlook for TNBC Patients with Insulin Resistance
- Part 7: FAQs About Insulin Resistance and Triple-Negative Breast Cancer
- Part 8: Final Thoughts
Foreword
A diagnosis of triple-negative breast cancer (TNBC) can raise many questions and uncertainties, especially when the connection between insulin resistance and TNBC is becoming more widely discussed. This rare and aggressive form of breast cancer presents unique challenges in treatment, and understanding how insulin resistance might play a role in its development can be an important step in finding better ways to approach care.

If you or a loved one is dealing with TNBC, it’s understandable to want to learn more about insulin resistance and how it affects both cancer growth and treatment. Researchers are increasingly uncovering the links between elevated insulin levels and cancer progression, particularly in cancers like TNBC, which are harder to treat due to their lack of hormone receptors.
In this article, we’ll explore the science behind insulin resistance, how it connects to TNBC, and what this means for current and future treatment strategies. We’ll also touch on the importance of lifestyle changes, such as diet and exercise, in managing insulin resistance and potentially improving outcomes for patients.
Understanding the links between metabolism and cancer growth opens new doors for treatment and offers hope that the future of cancer care may be more personalized than ever before.
Let’s begin by exploring what insulin resistance is, how it develops, and why it matters in the context of cancer.
Part 1: What Is Insulin Resistance?
When we talk about insulin resistance, we’re referring to a condition where your body’s cells stop responding properly to insulin, a hormone produced by the pancreas. Insulin plays a crucial role in regulating how your body processes sugarsand fats, so when it’s not working correctly, several things go awry. Insulin resistance can lead to higher-than-normal levels of insulin in the blood, which, over time, can contribute to type 2 diabetes and other serious health problems. But did you know that insulin resistance can also have an impact on cancer, including triple-negative breast cancer (TNBC)?
How Insulin Resistance Develops
In a healthy body, insulin helps regulate blood sugar levels by signaling cells to absorb glucose from the bloodstream. When you eat, especially foods high in sugar or carbohydrates, insulin helps shuttle that sugar into your cells, where it’s used for energy. However, if you have insulin resistance, your cells don’t respond to insulin as effectively. This means your body needs to produce more insulin to keep your blood sugar levels stable.
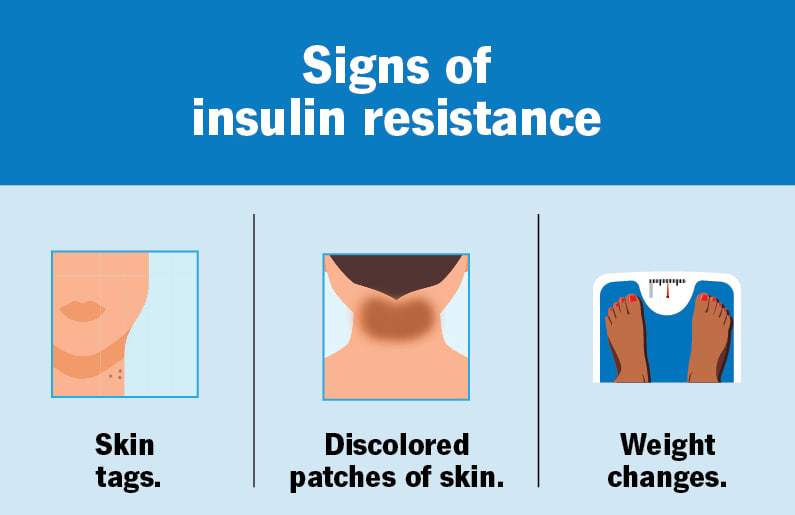
Several factors contribute to the development of insulin resistance, and it doesn’t happen overnight. Obesity, particularly excess belly fat, is one of the primary risk factors. Physical inactivity, poor diet, and even genetic factors can also play a role. Over time, as insulin resistance builds, your pancreas has to work harder to produce enough insulin. Eventually, this can lead to elevated insulin levels (known as hyperinsulinemia), and, if left unchecked, it can progress to type 2 diabetes.
Why Insulin Resistance Matters
You might be thinking, “Why should I care about insulin resistance?” The truth is, insulin resistance doesn’t just affect your blood sugar. Over time, it can disrupt several biological processes in your body that may have long-term effects. Elevated insulin levels have been linked to a variety of conditions, including:
- Type 2 diabetes: The most common outcome of prolonged insulin resistance, where your body can’t effectively manage blood sugar levels.
- Cardiovascular disease: High insulin levels can contribute to high blood pressure, high cholesterol, and increased risk of heart disease.
- Increased inflammation: Insulin resistance can trigger low-grade, chronic inflammation throughout the body, which is often a precursor to many diseases, including cancer.
One of the more concerning effects of insulin resistance is its connection to cancer, particularly triple-negative breast cancer (TNBC), a form of breast cancer that is more aggressive and harder to treat than other types. Studies have shown that high insulin levels may encourage the growth of cancer cells by affecting cell metabolism and increasing inflammation. This makes insulin resistance not just a metabolic concern but also a potential risk factor for developing certain cancers, including TNBC.
Part 2: What Is Triple-Negative Breast Cancer (TNBC)?
When you hear the term triple-negative breast cancer (TNBC), it’s referring to a specific subtype of breast cancer that doesn’t have three key markers that are typically present in more common forms of the disease. These markers are estrogen receptors, progesterone receptors, and HER2 (human epidermal growth factor receptor 2). In other words, triple-negative breast cancer is negative for all three of these markers. This is what makes it distinct, and also why it can be so challenging to treat.
The Characteristics of TNBC
Triple-negative breast cancer is often diagnosed as high-grade and aggressive, which means the cells look abnormal under a microscope and the cancer tends to grow and spread more quickly than other types of breast cancer. Since it lacks the hormone receptors and HER2, TNBC doesn’t respond to treatments like hormone therapy (which targets estrogen and progesterone receptors) or HER2-targeted therapy (like trastuzumab/Herceptin). These are two of the most common and effective treatments for other breast cancer types, so their absence leaves TNBC patients with fewer options for treatment.
TNBC tends to be more prevalent in younger women, African American women, and those with a BRCA1 gene mutation. It’s also more likely to occur in women who have a family history of breast cancer.
Why Is TNBC So Aggressive?
The aggression of TNBC can be attributed to several factors:
- Lack of targeted therapies: Without the presence of estrogen, progesterone, or HER2 receptors, TNBC cannot be treated with the therapies that are effective for other forms of breast cancer, such as tamoxifen or Herceptin. This lack of specific treatment options means that TNBC is typically treated with chemotherapy alone, which often comes with harsh side effects.
- Faster growth: TNBC is more likely to grow quickly, which means it can spread to other parts of the body, such as the lungs, liver, or bones, before it is detected. This rapid growth increases the chances of metastasis (the spread of cancer cells to other organs).
- Higher recurrence rates: After initial treatment, TNBC has a higher likelihood of recurrence within the first few years compared to other forms of breast cancer. This is particularly concerning for patients who may initially go into remission, only to see the cancer return aggressively.
Symptoms and Diagnosis
Like many forms of breast cancer, TNBC often presents as a lump or mass in the breast that can be detected through mammograms, ultrasounds, or MRI. Other possible symptoms include skin changes, such as redness or dimples on the breast surface, as well as pain or swelling in the breast or armpit area.
However, because TNBC is often diagnosed in later stages, it can be more difficult to treat and may require more intensive treatment strategies. Biopsy is essential to confirm the presence of TNBC and to assess the specific characteristics of the tumor. Pathologists will examine tissue samples to see if the cancer is negative for estrogen, progesterone, and HER2 receptors. This is the key step in diagnosing TNBC and distinguishing it from other breast cancers.
Treatment Challenges
The primary challenge with TNBC treatment lies in the lack of targeted therapies. Since TNBC is hormone receptor-negative and HER2-negative, conventional therapies that target these receptors are ineffective. The treatment plan typically involves a combination of chemotherapy, radiation, and, in some cases, surgery. Researchers are working to identify new treatment options for TNBC, including immunotherapies and targeted therapies that could make a significant difference in survival and quality of life.
Part 3: The Link Between Insulin Resistance and Triple-Negative Breast Cancer
The connection between insulin resistance and triple-negative breast cancer (TNBC) is an emerging area of research, one that could change how we approach treatment for this aggressive cancer. To understand how insulin resistance may contribute to the development and progression of TNBC, we need to explore the biological mechanisms at play and how they intersect with cancer cell behavior.
How Insulin Resistance Fuels Cancer Growth
Insulin resistance occurs when the body’s cells become less responsive to insulin, a hormone that helps regulate blood sugar levels. As a result, the body compensates by producing more insulin, leading to higher insulin levels in the bloodstream. While insulin’s primary job is to help cells absorb glucose, it also plays a key role in regulating other processes like cell growth, inflammation, and metabolism.
When insulin levels rise due to insulin resistance, it can trigger a series of reactions in the body that may fuel cancer growth. In TNBC, these effects are particularly concerning:
- Increased cell division: High levels of insulin can promote rapid cell division. For cancer cells, this means more opportunities for tumor growth and spread.
- IGF-1 activation: Insulin resistance is often accompanied by elevated levels of insulin-like growth factor 1 (IGF-1), a hormone that promotes cell growth and survival. IGF-1 can bind to receptors on cancer cells, stimulating their growth and making them more resistant to cell death (apoptosis). This makes the cancer more difficult to treat and more likely to spread.
- Chronic inflammation: Insulin resistance is associated with low-grade chronic inflammation throughout the body. Inflammation is a known cancer-promoting factor, as it creates an environment that supports tumor growthand metastasis (spread of cancer cells to other organs). The inflammation caused by insulin resistance can create a favorable environment for TNBC cells to grow and thrive.
Insulin and Tumor Metabolism
One of the key reasons why insulin resistance plays a significant role in cancer development is its effect on cell metabolism. Cancer cells, especially those in aggressive forms like TNBC, have altered metabolic pathways that allow them to survive and proliferate under challenging conditions. Insulin and IGF-1 are central to these altered metabolic processes.
- Energy production: Cancer cells often rely heavily on glucose for energy, a process known as aerobic glycolysisor the Warburg effect. Elevated insulin levels in insulin-resistant individuals can provide more glucose to fuel this process, supporting the growth of the cancer cells.
- Fat metabolism: Insulin resistance can also influence fat metabolism. The body tends to store more fat in response to insulin resistance, which not only increases the risk of obesity but also contributes to increased fatty acidscirculating in the bloodstream. These fatty acids can be used by cancer cells as an additional energy source, further promoting their growth.
The Role of Insulin Signaling Pathways in TNBC
At the molecular level, insulin resistance impacts the insulin signaling pathways that cancer cells use to regulate their growth and survival. These pathways are complex but can be broken down into a few key actions:
- Activation of the PI3K/AKT pathway: One of the major pathways influenced by insulin signaling is the PI3K/AKT pathway, which is involved in regulating cell growth, survival, and metabolism. Insulin resistance can hyperactivate this pathway, making cancer cells more resistant to treatment and promoting their proliferation.
- Activation of the mTOR pathway: Another important pathway influenced by insulin is the mTOR (mechanistic target of rapamycin) pathway. This pathway regulates cell growth and metabolism. In insulin-resistant individuals, mTOR is often overactive, which can contribute to tumor progression by promoting protein synthesis and cell growth.
- Tumor microenvironment: Insulin resistance can also alter the tumor microenvironment, making it more conducive to cancer growth. Elevated insulin levels increase angiogenesis (the formation of new blood vessels) to supply the tumor with oxygen and nutrients, aiding in the cancer’s growth and spread.
The Impact of Insulin Resistance on TNBC Outcomes
The link between insulin resistance and TNBC may also explain why individuals with insulin resistance or metabolic syndrome tend to have worse outcomes when it comes to TNBC. Elevated insulin levels, combined with the inflammatory environment they create, not only contribute to tumor growth but also make TNBC cells more resistant to chemotherapy and other treatments.
Several studies have shown that insulin resistance may contribute to poorer survival rates and higher rates of recurrence in TNBC patients. As TNBC is already a chemoresistant and aggressive cancer, the added complication of insulin resistance can make treatment even more challenging.
Part 4: How Insulin Resistance Affects TNBC Tumor Growth
Insulin resistance doesn’t just affect your body’s ability to regulate blood sugar; it can also play a significant role in how tumors, particularly in aggressive cancers like triple-negative breast cancer (TNBC), grow and spread. Understanding how insulin resistance influences tumor development helps explain why this cancer type is so difficult to treat and why patients with insulin resistance may experience worse outcomes.
Insulin and the Tumor Microenvironment
When insulin resistance occurs, the body’s elevated insulin levels create a tumor-friendly environment. High insulin levels promote angiogenesis, the process by which new blood vessels form. This is crucial because tumors, like all tissues, need an increased blood supply to grow and thrive. With more blood vessels feeding the tumor, it can receive more oxygen and nutrients, helping it grow faster and more aggressively.
Additionally, insulin resistance contributes to chronic inflammation in the body, which creates an environment where tumors are more likely to grow and spread. Inflammation is a well-known driver of cancer progression because it can promote cell survival and increase genetic mutations. Over time, this cycle of inflammation can push the tumor to become even more aggressive and resistant to treatments.
Altered Metabolism in Cancer Cells
Cancer cells are known to have altered metabolic pathways, and insulin resistance can exacerbate this. Insulin and insulin-like growth factors (IGF-1) influence tumor cell metabolism, encouraging cancer cells to use glucose and fatty acids as fuel for growth. Insulin resistance increases the amount of glucose circulating in the bloodstream, giving cancer cells more fuel to grow. This effect is especially significant in TNBC, which is already a fast-growing and aggressivecancer.
Additionally, insulin resistance can push cancer cells into a state where they rely more on fat metabolism, further supporting their rapid growth. This metabolic shift allows tumors to sustain themselves in environments where other cells might struggle, making them harder to treat.
Increased Tumor Invasion and Metastasis
Tumor cells in insulin-resistant individuals often show an increased tendency for invasion and metastasis, or the ability to spread to other parts of the body. Insulin resistance influences several pathways involved in these processes. It can promote epithelial-mesenchymal transition (EMT), a process that allows cancer cells to become more mobile, invade nearby tissues, and eventually spread to distant organs like the lungs, liver, or bones.
This ability to metastasize makes insulin-resistant individuals more likely to develop advanced-stage cancer and less likely to respond to conventional treatments like chemotherapy. The combination of insulin’s effects on metabolism, tumor microenvironment changes, and increased invasion makes TNBC tumors in insulin-resistant patients more difficult to control and more prone to spreading.
Insulin Resistance and Treatment Resistance
One of the biggest concerns with insulin resistance in TNBC is its impact on treatment effectiveness. Chemotherapy, a standard treatment for TNBC, works by targeting rapidly dividing cells. However, insulin resistance alters cancer cell metabolism, making them more difficult to target and destroy. Elevated insulin levels have been shown to help protect cancer cells from the effects of chemotherapy, making them more likely to survive and even develop resistance to drugs.
Moreover, insulin resistance may limit the effectiveness of other targeted therapies and hormonal treatments that rely on specific cancer cell markers. Since TNBC lacks the typical hormone receptors, and insulin resistance can influence gene expression, it can complicate treatment outcomes even further.
Part 5: Implications for Treatment
Understanding the link between insulin resistance and triple-negative breast cancer (TNBC) is crucial for developing more effective treatment strategies. Insulin resistance, as we’ve seen, can make TNBC more aggressive and harder to treat with conventional therapies. In this section, we’ll explore how this connection impacts current treatment options and what new strategies might be on the horizon to help improve outcomes for TNBC patients with insulin resistance.
Current Treatment Options for TNBC
Treating triple-negative breast cancer generally involves a combination of chemotherapy, surgery, and radiation therapy. Since TNBC lacks estrogen and progesterone receptors, and is HER2-negative, it doesn’t respond to standard hormonal therapies or HER2-targeted treatments, which are commonly used for other types of breast cancer. For this reason, chemotherapy remains the primary treatment option.
Chemotherapy
Chemotherapy drugs are often used to shrink tumors before surgery or to treat any remaining cancer cells afterward. Standard chemotherapy regimens for TNBC include doxorubicin, cyclophosphamide, taxanes (like paclitaxel or docetaxel), and carboplatin. While chemotherapy is effective for many patients, it can be less effective for those with insulin resistance because the elevated insulin levels can promote tumor growth and help cancer cells survive treatment.
Research into combining chemotherapy with therapies aimed at addressing insulin resistance could be an important next step in improving the effectiveness of these drugs. For example, drugs like metformin, commonly used to treat type 2 diabetes and insulin resistance, are being explored as potential adjunct therapies for cancer treatment.
Surgery and Radiation
Surgical options like mastectomy or lumpectomy are typically performed to remove the tumor. Depending on the stage and location of the tumor, radiation therapy might be used after surgery to eliminate remaining cancer cells and reduce the risk of recurrence. While these treatments are necessary, the presence of insulin resistance can increase the risk of cancer recurrence, making it more important to manage insulin levels and other factors during treatment.
Targeting Insulin Resistance as Part of Cancer Treatment
One promising approach is to target insulin resistance directly as part of the treatment plan. By addressing insulin resistance, doctors may be able to reduce the cancer-promoting effects of elevated insulin and improve the body’s response to treatment.
Metformin: A Potential Game Changer
Metformin, a drug commonly prescribed for managing type 2 diabetes, is one of the most studied treatments for insulin resistance in the context of cancer. Metformin works by improving the body’s sensitivity to insulin and lowering insulin levels, which could potentially reduce the growth and spread of TNBC tumors.
In addition to its effects on insulin, metformin has shown potential in directly inhibiting cancer cell growth by affecting key cancer-related pathways, including the mTOR pathway, which is involved in cell growth and survival. Some studies suggest that metformin could be a valuable addition to traditional cancer treatments, especially for patients who have insulin resistance.
While metformin is not yet a standard treatment for TNBC, it’s being actively studied in clinical trials to assess its effectiveness in improving outcomes for patients with TNBC and insulin resistance. If proven effective, it could be a game-changer in the management of TNBC, offering a dual benefit of controlling both insulin resistance and cancer growth.
Lifestyle Interventions: Exercise and Diet
In addition to medications like metformin, lifestyle changes can have a significant impact on insulin resistance and cancer outcomes. Engaging in regular physical activity and adopting a healthy diet are key strategies for improving insulin sensitivity. Research has shown that even modest weight loss and increased exercise can help lower insulin levels, potentially reducing the growth of TNBC tumors.
While lifestyle interventions alone are unlikely to replace standard cancer treatments, they can complement chemotherapy, radiation, and other therapies by improving the overall metabolic environment and reducing inflammation in the body. These changes may also help reduce the risk of recurrence, improve quality of life, and make the body more receptive to treatment.
Emerging Therapies: Combining Insulin Resistance Management with Cancer Treatment
As more is learned about the relationship between insulin resistance and TNBC, new therapeutic strategies are being explored. The combination of insulin resistance management with targeted cancer therapies represents a promising frontier in cancer treatment. Future research may lead to the development of drugs that can lower insulin levels while also targeting specific cancer pathways, offering more effective and less toxic treatment options.
Part 6: Prognosis and Outlook for TNBC Patients with Insulin Resistance
If you’ve been diagnosed with triple-negative breast cancer (TNBC) and have insulin resistance, you might be wondering how both factors affect your prognosis and treatment options. While TNBC is already known for being an aggressive and difficult-to-treat cancer, the presence of insulin resistance can add another layer of complexity to the situation. However, understanding this connection can also offer new opportunities for treatment and improvement.
Impact of Insulin Resistance on Prognosis
Insulin resistance can worsen the prognosis of TNBC by contributing to tumor growth, metastasis, and resistance to treatment. Elevated insulin levels, caused by insulin resistance, can promote the growth of cancer cells by activating cell survival pathways and increasing inflammation. This makes it more likely that the cancer will grow and spread faster than it would in a patient without insulin resistance.
In addition to fueling cancer progression, insulin resistance can also impair the effectiveness of standard cancer treatments, such as chemotherapy. Since insulin resistance promotes tumor growth and cell survival, cancer cells are more likely to survive chemotherapy and other treatments, which means there may be higher rates of recurrence and poorer survival outcomes for TNBC patients with insulin resistance.
However, the impact of insulin resistance on prognosis doesn’t have to be all bad news. By managing insulin resistance effectively, it may be possible to improve treatment outcomes, reduce tumor growth, and lower recurrence rates. Addressing insulin resistance through lifestyle changes or medications like metformin could offer a way to improve the chances of successful treatment, though more research is needed to confirm the full extent of these benefits.
Treatment Response and Insulin Resistance
The presence of insulin resistance may also affect how a TNBC patient responds to chemotherapy and radiation therapy. As insulin resistance can help cancer cells survive and proliferate, it can make chemotherapy less effective, leading to treatment resistance. This makes it crucial to consider additional therapies that can address both insulin resistance and tumor growth.
Metformin, for example, is currently being studied for its potential to improve chemotherapy outcomes by not only managing insulin resistance but also directly targeting cancer cells. Early research shows promise, indicating that combining insulin resistance management with chemotherapy may improve the overall response to treatment and reduce the risk of metastasis.
Additionally, insulin resistance’s impact on tumor metabolism makes it important to consider targeted therapies and personalized treatment plans. By identifying specific genetic or metabolic factors involved in a patient’s cancer, doctors may be able to craft a treatment strategy that is more effective than standard chemotherapy alone.
Improving Prognosis through Lifestyle Changes
Managing insulin resistance through lifestyle interventions can also play a significant role in improving the prognosis for TNBC patients. Research has shown that weight loss, regular exercise, and a healthy diet can improve insulin sensitivity and reduce elevated insulin levels. Even modest changes in lifestyle, such as losing a small amount of weight and increasing physical activity, can help reduce the tumor-promoting effects of insulin resistance.
Lifestyle changes not only help with insulin sensitivity but can also improve overall health, making it easier to tolerate cancer treatments. For example, regular physical activity has been shown to improve immune function, reduce inflammation, and enhance chemotherapy effectiveness, all of which can positively affect the treatment outcomes for TNBC patients.
Though lifestyle changes alone cannot replace traditional treatments, they can be an important part of an integrated approach to managing TNBC. With the right combination of exercise, diet, and medication, patients can potentially improve their response to treatment and reduce the risk of cancer recurrence.
Hope for the Future
While the prognosis for TNBC patients with insulin resistance may be more challenging, there is hope on the horizon. Ongoing research into personalized treatments and immunotherapies holds great potential for improving outcomes for patients with both TNBC and insulin resistance. The focus on understanding the biological mechanisms linking insulin resistance to cancer progression is opening up new opportunities for more effective therapies, particularly those that address both metabolism and cancer growth.
Additionally, clinical trials are playing a crucial role in exploring how medications like metformin, lifestyle changes, and combination therapies can improve survival rates and quality of life for TNBC patients. By participating in these trials, patients have access to cutting-edge treatments that may offer more promising results than traditional options.
Part 7: FAQs About Insulin Resistance and Triple-Negative Breast Cancer
Understanding how insulin resistance impacts triple-negative breast cancer (TNBC) can raise many questions. Below, we’ve gathered some of the most frequently asked questions to help provide more clarity about this connection and how it affects treatment, prognosis, and overall health.
1. What is insulin resistance, and how does it relate to cancer?
Insulin resistance occurs when the body’s cells become less responsive to insulin, leading to higher insulin levels in the bloodstream. This can result in elevated glucose and fatty acid levels, which can fuel tumor growth. In the case of triple-negative breast cancer (TNBC), insulin resistance may promote cancer cell survival, growth, and metastasis, making it harder to treat. Insulin and insulin-like growth factor (IGF-1) play key roles in these processes, helping the cancer cells thrive and evade treatment.
2. Can managing insulin resistance improve treatment outcomes for TNBC patients?
Yes, managing insulin resistance can improve treatment outcomes. When insulin levels are controlled, it helps reduce cancer-promoting effects, such as tumor growth and inflammation. Medications like metformin, which are used to treat insulin resistance in type 2 diabetes, are currently being researched to see if they can also improve the effectiveness of chemotherapy for TNBC patients. In addition, lifestyle changes such as exercise and a healthy diet can improve insulin sensitivity, making the body more responsive to treatment.
3. Can lifestyle changes help manage insulin resistance in TNBC patients?
Absolutely. Lifestyle modifications play a significant role in managing insulin resistance. Regular exercise, a balanced diet, and weight management can help improve insulin sensitivity, reduce insulin levels, and lower the risk of cancer progression. Even modest changes, such as losing a small amount of weight or increasing physical activity, can make a big difference in how the body handles insulin and responds to treatment.
4. Is insulin resistance more common in TNBC patients?
Research suggests that insulin resistance may be more common in TNBC patients, particularly those who have metabolic syndrome, which includes factors like obesity, high blood pressure, and high cholesterol. Obesity, in particular, is a known risk factor for both insulin resistance and the development of TNBC. However, while insulin resistance is prevalent in certain TNBC patients, it’s not present in all cases. The relationship between metabolic factorsand cancer is still an area of active research.
5. How does insulin resistance affect chemotherapy effectiveness in TNBC?
Insulin resistance can make chemotherapy less effective for TNBC patients. Elevated insulin levels promote tumor survival and resistance to chemotherapy, making cancer cells more likely to survive and grow despite treatment. This is why researchers are exploring combination therapies that address both insulin resistance and cancer growth, such as adding metformin to chemotherapy. By targeting both the cancer cells and the metabolic pathways that support them, these treatments may improve overall effectiveness.
6. What is metformin, and can it help TNBC patients with insulin resistance?
Metformin is a medication commonly used to treat type 2 diabetes by improving the body’s response to insulin. Recent studies suggest that metformin may have additional benefits for cancer patients, including those with TNBC. Metformin has been shown to lower insulin levels and inhibit cancer cell growth, making it a promising candidate for TNBC treatment. Clinical trials are ongoing to evaluate whether metformin can improve treatment outcomes for TNBC patients with insulin resistance.
7. Are there any new treatments being researched for TNBC and insulin resistance?
Yes, ongoing research is exploring new treatments that target both insulin resistance and cancer growth in TNBC patients. Medications like metformin are being tested in combination with chemotherapy and immunotherapy to see if they can improve response rates and overall survival. Additionally, targeted therapies and personalized treatment plans that take both metabolic factors and cancer characteristics into account are also being explored. Clinical trials are crucial in advancing these treatments, offering hope for more effective therapies in the future.
Part 8: Final Thoughts
The connection between insulin resistance and triple-negative breast cancer (TNBC) offers important insights into how we might approach treatment for this aggressive form of cancer. While TNBC is known for being hard to treat due to its lack of hormone receptors and its rapid growth, the role of insulin resistance provides an opportunity to look at new treatment strategies and better ways to manage the disease.
Though insulin resistance can make cancer more difficult to treat, the good news is that it’s manageable. Lifestyle changes, like dietary adjustments and increased physical activity, can have a significant impact on controlling insulin levels, potentially reducing the growth of tumors. Medications like metformin, commonly used to treat type 2 diabetes, are showing promise in clinical trials as a way to manage both insulin resistance and cancer progression. This is an exciting development because it means we could one day treat both the metabolic condition and the cancer at the same time.
In the meantime, patients with TNBC should work closely with their healthcare providers to develop a personalized treatment plan. This plan might include chemotherapy, radiation therapy, and supportive treatments to help manage the side effects. Additionally, targeted therapies and immunotherapies are becoming more prominent in cancer care, offering hope for better outcomes, particularly in patients with insulin resistance.
It’s also important to remember that the fight against TNBC is ongoing. With advancements in research and clinical trials, more effective treatments and early detection methods are on the horizon. If you or a loved one has been diagnosed with TNBC, it’s vital to stay informed, ask questions, and explore all available treatment options. Don’t hesitate to seek support from healthcare professionals, support groups, or mental health counselors to ensure you’re getting the comprehensive care you need.
In conclusion, while TNBC remains a difficult and challenging cancer to treat, understanding its relationship with insulin resistance opens up new avenues for improving care and survival outcomes. The future is bright, with researchoffering the potential for better, more personalized treatments for those affected by this aggressive cancer.









