60 Percent VA Rating for Prostate Cancer: Eligibility and Benefits
- Foreword
- 1. Introduction to VA Disability Ratings
- 2. Understanding Prostate Cancer in Veterans
- 3. VA Rating Criteria for Prostate Cancer
- 4. Achieving a 60% VA Rating: Eligibility and Criteria
- 5. Service Connection: Establishing the Link
- 6. Navigating the VA Claims Process
- 7. Special Monthly Compensation (SMC) and Additional Benefits
- 8. Common Challenges and How to Overcome Them
- 9. Resources and Support for Veterans
- 10. Frequently Asked Questions (FAQ)
- 11. Closing Thoughts
Foreword
If you’re a veteran dealing with prostate cancer—or helping someone who is—then you already know that navigating the VA system can feel like trying to read fine print in a dark room. You’ve served your country, and now you’re simply asking for what’s fair: recognition, support, and compensation for a condition that may well be tied to your service. But the rules around disability ratings? The numbers, percentages, legal phrases, and paperwork? That part can feel anything but fair.
This guide is here to change that. We’re going to talk specifically about what it means to receive a 60 percent VA disability rating for prostate cancer. That number—60—isn’t random. It can mean the difference between a life of financial strain and one where you get the breathing room to focus on your health and quality of life. It also opens the door to other benefits you might not even know you’re eligible for.
But let’s start with the bigger picture: What even is a VA disability rating? Who decides it, and why do prostate cancer ratings change over time? Why do some veterans get 100 percent while others—perhaps with similar symptoms—receive far less?
If those questions are on your mind, you’re not alone. The VA’s rating system can feel opaque, but there is a logic to it. And once you understand that logic, you’re in a better position to advocate for yourself, gather the right documentation, and challenge decisions that don’t reflect your reality.
So let’s dig in—starting with the foundation: how the VA disability rating system actually works, and why understanding it is key to getting what you deserve.
Introduction to VA Disability Ratings
You’ve probably heard phrases like “VA compensation,” “disability rating,” or “service connection” thrown around, sometimes by other veterans, sometimes by the VA itself. But what do they actually mean?
At its core, a VA disability rating is a number—expressed as a percentage from 0 to 100—that reflects how much a service-connected condition affects your ability to function in daily life and work. The higher the rating, the greater the presumed impact on your earning capacity and overall quality of life, and the higher the monthly compensation you receive from the VA.
So when someone says they have a 60% rating, they’re saying the VA has officially recognized that their service-connected health issue reduces their capacity to function by 60%. That’s not just an abstract number—it translates into a specific dollar amount each month and opens the door to additional benefits, including healthcare eligibility, tax breaks, and more.
But here’s where it gets tricky: prostate cancer is not rated like many other conditions.
When prostate cancer is active—meaning it’s being treated with surgery, radiation, hormone therapy, or other methods—the VA typically assigns a 100% temporary rating. That’s because the disease and its treatments are considered totally disabling. But once treatment ends and the cancer goes into remission, the VA reevaluates. That’s when most veterans see their rating drop—to 60%, 40%, 20%, or even 0%, depending on the residual symptoms left behind.
So where does the 60% rating come in?
This is the sweet spot for many veterans who are no longer in active treatment but are still dealing with serious, disruptive symptoms. The VA’s rating schedule takes into account things like urinary incontinence, the need for absorbent materials, and the use of appliances like catheters. If your symptoms are severe enough to meet specific criteria—say, needing to change absorbent pads more than four times a day—you may qualify for that 60% rating.
But here’s a question worth asking: Is the VA always accurate in assigning these ratings? Unfortunately, no. Many veterans are underrated, either because they don’t know what evidence to submit, weren’t properly evaluated, or simply didn’t realize their symptoms could qualify them for more.
This is why understanding the VA’s rating system isn’t just useful—it’s strategic. It puts you in control. It helps you build a claim that speaks the VA’s language while telling your truth.
This guide often pairs well with general overviews like VA Ratings for Cancer in Remission, which puts the 60% figure in broader context.
In the next section, we’ll take a closer look at why prostate cancer affects veterans at higher rates, what symptoms matter most when the VA decides your rating, and how to ensure those symptoms are seen, heard, and counted. If you’ve ever felt like your rating doesn’t match your reality, you’ll want to keep reading.
Understanding Prostate Cancer in Veterans
Let’s step back for a moment and talk about the condition itself—prostate cancer. Not the paperwork, not the VA process, but the actual medical reality behind the diagnosis.
Why prostate cancer? Why is it such a frequent visitor in the lives of veterans?
The short answer: exposure. The longer answer: a mix of aging, service-related environmental factors, and, for some, a toxic legacy like Agent Orange. Prostate cancer is one of the most commonly diagnosed cancers in men overall, but among veterans—particularly those who served in Vietnam, Korea, or certain parts of Southeast Asia—the rates are disproportionately high. So if you’re wondering, “Was it just bad luck?”—that’s not the whole story. The VA acknowledges that certain military exposures increase the risk of prostate cancer. And that acknowledgment matters, because it helps establish what the VA calls a presumptive service connection—which we’ll break down later.
But before we get to the legal side of things, let’s be clear about what this disease does to the body—and why its effects can linger long after the cancer is technically “gone.”
What happens during and after prostate cancer?
The prostate is a small gland, but when cancer takes hold, the impact is rarely small. The treatments—surgery, radiation, hormone therapy—can be life-saving, yes. But they can also leave behind a long list of complications. And here’s the catch: those complications are what the VA often bases your long-term disability rating on.
So what kind of symptoms are we talking about?
- Urinary incontinence – A common result of prostate removal (prostatectomy) or radiation, this can range from occasional dribbling to full loss of bladder control. Some veterans need to wear absorbent pads. Others rely on medical appliances. And this isn’t just inconvenient—it can be isolating, anxiety-inducing, and physically uncomfortable.
- Erectile dysfunction (ED) – Another major aftereffect of prostate cancer treatment. The nerves and blood vessels that control erection often run close to the prostate. When surgery or radiation damages them, ED can become permanent. While the VA often assigns a “0% rating” for ED, it’s still considered a compensable condition in the form of Special Monthly Compensation (SMC)—which we’ll unpack later.
- Frequent urination, urgency, and nocturia – You might find yourself needing to urinate every hour, or waking up several times a night. This might seem minor to some people. It’s not. Over time, it can grind down your sleep, energy levels, and overall well-being.
- Bowel issues and pelvic pain – Less common, but not rare, especially for veterans who underwent pelvic radiation. Chronic pain or bowel dysfunction can be just as disabling as the more widely discussed symptoms.
Now let’s ask the obvious question: If my cancer is in remission, why does the VA still rate me at all?
Because remission doesn’t mean recovery. Not in the full sense. The VA recognizes that even when the cancer is “cured” or in remission, the aftermath can be disabling in itself. That’s why the VA looks beyond the word “remission” and focuses on what’s left behind—residual symptoms.
And that’s the key to understanding how a 60% rating can still apply long after your last radiation session or surgery. The VA isn’t (or isn’t supposed to be) rating the diagnosis. It’s rating the functional impact of the condition as it exists today.
So if you’re someone who’s had their prostate cancer treated, maybe even years ago, and you’re still changing pads multiple times a day or dealing with daily ED, you are absolutely still entitled to compensation. But as we’ll explore, getting that compensation depends on whether the VA is properly recognizing and categorizing your symptoms.
Here’s another question you might be asking: How does the VA determine whether my symptoms are worth 20%, 40%, or 60%?
The answer lies in something called Diagnostic Code 7528 under the VA’s Schedule for Rating Disabilities. It’s basically the playbook the VA uses to assign ratings. We’ll dive deep into that in the next section—because understanding the rules of that playbook is how you play the game.
But for now, just know this: your experience is valid, and your symptoms matter. You didn’t just “get old” or “get unlucky.” You got cancer. You got treated. And now you’re living with the cost. The VA is supposed to help carry that cost. Let’s make sure they do.
VA Rating Criteria for Prostate Cancer
So now we arrive at the part where the VA assigns a number to what you’ve been through. It’s impersonal, bureaucratic, and—to be blunt—often frustrating. But it’s also how the system works. And if you understand the criteria the VA uses, you’re in a far better position to advocate for yourself.
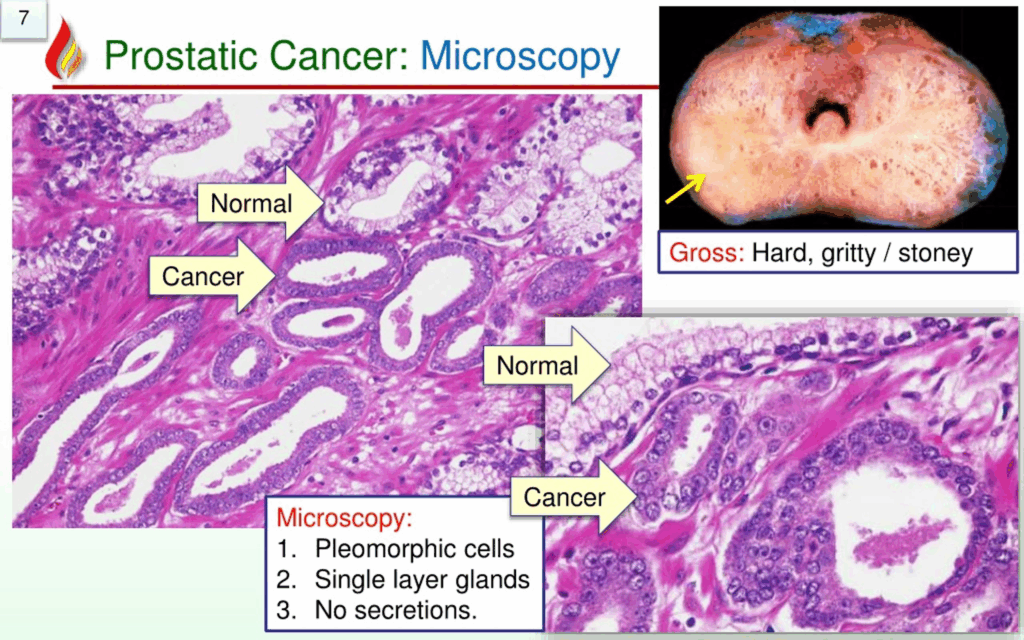
Let’s start with this: the VA does not assign one static rating for prostate cancer. Your rating can—and often will—change over time, depending on where you are in the treatment and recovery process.
Sound confusing? It is. But it follows a certain logic once you know the rules.
The 100% Rating: While Cancer is Active
If you’re undergoing treatment for prostate cancer—whether it’s surgery, radiation, hormone therapy, or chemotherapy—you qualify for a temporary 100% disability rating. This isn’t up for debate. It’s automatic under Diagnostic Code 7528, which governs “malignant neoplasms of the genitourinary system.”
Why? Because cancer treatment, especially for something as serious as prostate cancer, is considered totally disabling by default. You’re in the thick of the fight, and the VA acknowledges that.
Here’s the fine print: the 100% rating remains in effect for the duration of the treatment and continues for six months after the treatment ends. That’s the buffer period. The VA assumes that even when treatment ends, your body and life are still very much in recovery mode.
Then comes what’s known as a mandatory re-evaluation.
The Post-Treatment Evaluation: Down Goes the Rating
About six months after your last cancer treatment, the VA will schedule a Compensation & Pension (C&P) exam to determine whether your cancer is in remission and what—if any—residual symptoms remain.
This is the part that catches many veterans off guard.
If your PSA levels are stable and there’s no evidence of recurrence, the VA considers your cancer “cured” (for disability purposes). But that’s when your rating often drops dramatically. How much it drops depends entirely on those residual effects we talked about in the last section—especially urinary dysfunction and erectile dysfunction.
Let’s focus on the most important part for our purposes: urinary incontinence, because this is where the 60% ratingoften comes into play.
The 60% Rating: Not Active Cancer, But Still Major Impact
According to the VA’s rating schedule under Diagnostic Code 7527 and 7528, a 60% disability rating can be assigned if:
- You require the use of an appliance (like a catheter),
or - You must change absorbent materials more than four times per day.
Think about that: four full pad changes, every single day. The VA treats this level of incontinence as severely disabling—and rightly so. It affects your freedom to travel, to work, to sleep, to live without fear of leakage or discomfort.
Now, if you’re changing pads three times a day, you may fall under a 40% rating. If it’s only once or twice a day, that could be 20%. And if your incontinence is mild or easily controlled? Possibly 0%. It’s a sliding scale, and where you land depends on how well your symptoms are documented—in your own words, in your doctor’s notes, and during your C&P exam.
Erectile Dysfunction: A Tricky Case
Now let’s touch on something that the VA doesn’t rate as generously: erectile dysfunction (ED). Almost every veteran who undergoes treatment for prostate cancer will experience some degree of ED. It’s not an exception—it’s the norm. But here’s the VA’s take: ED alone doesn’t impair your ability to work, so it’s often assigned a 0% disability rating.
Sound unfair? It is—until you realize there’s a workaround.
That workaround is called Special Monthly Compensation (SMC) – specifically SMC(k). This is an additional monthly benefit provided when you experience “loss of use of a creative organ.” In layman’s terms: if prostate cancer or its treatment leaves you impotent, you may be eligible for this compensation—even if the ED itself is rated at 0%.
So, even if the VA minimizes the severity of ED in its rating system, it doesn’t mean you go uncompensated. You just have to apply through a slightly different path.
What If I Still Have Active Cancer?
A fair and frequently asked question: What if I’m still receiving treatment, but the VA reduced my rating anyway? That shouldn’t happen. If your cancer is still active—or if you’ve had a recurrence—you should remain at the 100% rating level. But administrative mistakes happen. Ratings sometimes get dropped early, before that six-month post-treatment window closes, or even before treatment is completed.
If that’s the case, you have the right to file for a rating increase or submit a Notice of Disagreement (NOD) to challenge the decision.
One Last Important Point: Don’t Self-Minimize
Many veterans are conditioned—by military culture, by habit, by sheer grit—to underreport their symptoms. If you downplay how often you need to change pads, or gloss over your incontinence because you don’t want to seem “weak,” the VA takes you at your word. And that can cost you thousands in lifetime compensation.
Being honest about what you’re experiencing isn’t complaining. It’s documenting.
If you’re dealing with testicular concerns as well, this piece on low testosterone in testicular cancer covers a related diagnostic landscape.
Achieving a 60% VA Rating: Eligibility and Criteria
Let’s get tactical.
At this point, you know the VA disability rating for prostate cancer can drop significantly after treatment ends—and you know that 60% is one of the highest residual ratings possible if the cancer is in remission. But what exactly does it take to secure that 60% rating? How do you prove that your day-to-day reality still meets the criteria, even if your cancer is no longer “active”?

More importantly: Why do so many veterans fall short of that 60%, even when they should qualify?
Spoiler: It’s rarely because their symptoms aren’t serious enough. It’s usually because the symptoms weren’t properly documented, described, or linked to the right rating criteria in the VA’s internal playbook. This section is going to change that.
First, a quick refresher: what earns 60%?
Under the VA’s rating schedule for genitourinary conditions, particularly the diagnostic codes tied to residuals of prostate cancer, a 60% rating is warranted if:
- You require the use of an appliance for urinary control
OR - You must change absorbent materials more than four times per day
That sounds simple. But of course, nothing is ever that simple with the VA.
Let’s unpack those two key qualifiers.
What counts as an “appliance”?
When the VA says “appliance,” they don’t mean a refrigerator. They mean medical devices used to manage urination—like catheters. If you are using an indwelling catheter, intermittent catheterization, or any external urinary device (such as a urostomy bag or condom catheter), that should qualify. It’s not about the inconvenience of using it—it’s about the fact that your bladder no longer functions normally without external help.
One common issue: medical records may not explicitly use the word “appliance.” Instead, your doctor might just note the name of the device. If the VA rater doesn’t recognize that as an “appliance,” your claim could be underrated. That’s why it helps to spell it out clearly in your statement: “I require the use of a [device], which is an appliance used for urinary control.”
You have to connect the dots for them.
And what about absorbent materials?
This is the area most veterans rely on when aiming for a 60% rating. The question the VA asks is: How many times per day do you need to change pads or other absorbent materials?
The key thresholds are:
- 1–2 times/day = 20%
- 2–4 times/day = 40%
- More than 4 times/day = 60%
Seems straightforward, right? Here’s where things get sticky.
The VA won’t take your word alone. If you say, “I change pads five times a day,” they want to see corroborating evidence. That could be:
- A doctor’s note confirming the frequency
- A bladder diary that tracks how often you change pads over a week or more
- Statements from your spouse or caregiver
- Your own detailed written statement explaining your daily routine, including how often pads are changed, how full they get, and how this affects your ability to work, travel, sleep, and socialize
Don’t just say, “I use five pads.” Explain why. Describe what happens if you don’t. Detail the leaks, the accidents, the clean-ups, the fear of going places without a bathroom nearby. Make it real.
Because if you don’t spell it out, the VA won’t fill in the blanks for you.
Pro tip: Don’t trust the C&P exam alone.
Your Compensation & Pension (C&P) exam is a major part of the VA’s decision-making process. But let’s be honest—some of these exams are five-minute drive-thrus. If the examiner doesn’t ask about pad use, or you’re too modest to elaborate, you may leave that room without giving them the full picture.
So should you exaggerate? Absolutely not. But you should prepare.
Before the exam, write down a detailed symptom summary. Better yet, bring your bladder diary. And if they don’t ask about your urinary frequency or pad usage, offer it anyway. This is your one shot to tell your story in the language the VA uses to determine benefits.
And if the examiner gets it wrong—say, they note “two pad changes” when you said five—you can challenge it. You can submit a written rebuttal after the fact. You can get an outside doctor to write a clarifying statement. You can file for a higher-level review. You are not stuck.
What if your symptoms vary?
This is an important nuance. Many veterans don’t experience exactly the same symptoms every day. You might have a few days where you only need two pads. Then a day where you go through six. So what does the VA want? Consistency? Averages? Extremes?
They look at overall frequency and impact. If your normal, most typical day involves four or more pad changes, that’s your baseline. But even if you fluctuate, don’t assume you’re disqualified. If your symptoms ever rise to the level of requiring more than four daily changes on a recurring basis, you have a case to make.
Document those fluctuations. Explain what triggers the bad days. Be thorough.
Bonus value: Secondary conditions
Another strategic way to strengthen your case is to connect secondary conditions to your prostate cancer.
For example:
- Depression or anxiety due to ED? That’s a ratable mental health condition.
- Skin irritation or infections from chronic pad use? That’s a secondary physical condition.
- Sleep disturbances from constant nighttime urination (nocturia)? That can contribute to a case for Total Disability based on Individual Unemployability (TDIU), which we’ll discuss later.
In short: the VA must consider everything your service-connected condition causes—not just the cancer itself.
The big takeaway
Veterans who qualify for a 60% rating often miss out—not because they didn’t suffer enough, but because the paperwork didn’t tell the whole truth. The burden of proof lies with you, but the tools are in your hands: consistent tracking, medical corroboration, clear statements, and the willingness to push back if something feels off.
Next, we’ll explore how to link your cancer to your service—whether through direct evidence or VA-recognized presumptions—so you can establish that critical first step: service connection. Because before the VA will assign any rating at all, they need to be convinced your cancer isn’t just unfortunate—it’s service-related.
Service Connection: Establishing the Link
Before the VA gives you a single percentage point—whether it’s 60% or 100%—they need to answer one question first: Is your prostate cancer connected to your military service? If the answer is yes, you’re in the game. If not, it doesn’t matter how severe your symptoms are—the VA won’t rate the condition at all.
That may sound frustrating, especially if you’re thinking, “I served. I got cancer. What more proof do they need?” But from the VA’s standpoint, they aren’t just looking for a diagnosis—they’re looking for a service connection. And that’s a legal standard, not a medical one.
So, let’s break it down.
In VA terms, service connection means your prostate cancer either began during your military service, was caused by something that happened during service, or can be presumed to be related to your service because of known exposures or environmental risks. That last part—presumptive service connection—is the path most veterans take when it comes to prostate cancer, and it’s a powerful one.
If you served in Vietnam, Thailand, certain parts of Korea, or on ships that operated in Vietnam’s territorial waters during specific years, the VA assumes you were exposed to Agent Orange—a toxic herbicide used extensively during the Vietnam War. And guess what? Prostate cancer is one of the conditions that the VA presumes is caused by Agent Orange exposure. That means you don’t have to prove the cancer was caused by the chemical—you just need to prove you were in a location where the exposure occurred and that you now have the diagnosis. The dots connect themselves.
There are other recognized exposure categories too, like certain radiation exposure scenarios. If you were involved in nuclear testing or served near known contaminated sites, your claim may fall into that category. But for most veterans dealing with prostate cancer, Agent Orange is the most straightforward presumptive route.
Now, what if you don’t qualify for a presumptive connection?
Then you’ll need to go the direct service connection route, which takes a little more effort but is absolutely possible. You’ll need three things:
- A current diagnosis of prostate cancer (or its residuals),
- Evidence of an in-service event, exposure, or incident that could plausibly relate to the cancer, and
- A medical nexus opinion—a written statement from a qualified medical professional stating that your prostate cancer is “at least as likely as not” (a 50/50 chance) connected to your service.
That phrase—“at least as likely as not”—isn’t just a formality. It’s the VA’s gold standard for linking a condition to service. If a doctor can explain how your military exposure or service environment reasonably contributed to your cancer, that’s often enough to establish the link.
Don’t forget: lay evidence can help too. You can submit a personal statement describing symptoms that began during or shortly after service, or buddy statements from those who witnessed your condition or exposure. These don’t replace medical evidence, but they can support it.
Now let’s address a common concern: “My cancer didn’t show up until decades after I left the military—does that ruin my case?” Thankfully, no. The VA understands that some service-connected conditions, especially cancers, don’t show up right away. That’s why presumptive service connections exist—to acknowledge delayed onset diseases tied to exposure.
If your claim is denied or the VA refuses to recognize the service connection, don’t panic. You have options: file a supplemental claim with new evidence, request a higher-level review, or take your case to the Board of Veterans’ Appeals. Many strong claims are initially denied—not because the veteran doesn’t qualify, but because the evidence wasn’t framed the right way.
Here’s the bottom line: you don’t have to prove the military caused your cancer with 100% certainty. You just have to show it’s as likely as not. Whether that’s through presumptive exposure or a strong medical opinion, this is the foundation your entire claim will stand on. So take your time. Get the right help. And make your case count.
Navigating the VA Claims Process
ALet’s talk about the nuts and bolts: filing your VA claim. You’ve got the diagnosis, you understand how ratings work, and maybe you’ve even nailed down your service connection. But now you’re staring at a form—or maybe a blinking cursor on VA.gov—and thinking, “How do I actually get this through the system?”
That’s what this section is for. Because no matter how solid your case is, if it’s not filed properly, it can stall or sink before it ever gets evaluated.
Step One: Filing the Claim
The most common way to start your VA claim is online through VA.gov or eBenefits. It’s relatively user-friendly, and it lets you upload documents, track your claim, and submit forms electronically. But there are other routes, too. You can file your claim in person at a VA regional office, or—better yet—with the help of a Veterans Service Organization (VSO).
VSOs like the VFW, DAV, American Legion, and others have accredited reps who specialize in helping veterans navigate the system. And here’s the best part: they’ll help you for free. If you’ve never filed a VA claim before—or if your last one didn’t go well—get a VSO in your corner. They know how to phrase things, what the VA looks for, and where people tend to trip up.
Step Two: Gathering Documentation
A successful claim is built on evidence. The more specific and well-documented your condition is, the easier it is for the VA to grant you the rating you deserve.
Here’s what you’ll want to pull together:
- Your DD-214 or other discharge paperwork
- Private and/or VA medical records showing your prostate cancer diagnosis, treatment, and current symptoms
- A nexus letter (if you’re not using a presumptive service connection)
- A personal statement describing how your symptoms affect your life—how many pads you use per day, how often you wake up to urinate, whether you use appliances, and so on
- Buddy statements, if applicable, from family or friends who witness your condition daily
The goal? Paint a clear, undeniable picture of what your condition really looks like day-to-day.
Step Three: The C&P Exam
Ah yes—the infamous Compensation & Pension (C&P) exam. If the VA needs more information, they’ll schedule this exam to evaluate your condition and residuals. Don’t take this lightly. What happens during this appointment can make or break your rating.
Here’s what to do:
- Prepare ahead of time. Write down your symptoms, how often you change pads, whether you use a catheter, how often you have accidents. Bring notes if you need to.
- Don’t hold back. Many veterans—out of pride, conditioning, or nerves—minimize their symptoms. Don’t. Be honest. Be thorough. Be clear.
- Follow up. If something was missed or misrepresented in your exam report, you have the right to submit a rebuttalor additional evidence.
Think of the C&P exam as your opportunity to speak directly to the person writing the first draft of your disability rating. Make sure they get the full picture.
Step Four: Waiting and Watching
Once your claim is submitted and your C&P exam is complete, you’ll enter the VA’s decision phase. This can take several months, sometimes longer. You can check the status online, and if your case is moving slowly, don’t be afraid to call the VA or ask your VSO for updates.
Remember: slow doesn’t mean doomed. The VA handles an enormous volume of claims. If yours is well-documented and well-supported, it’ll rise to the top in time.
Step Five: What If They Get It Wrong?
Let’s be real—sometimes the VA lowballs your rating, or denies the claim altogether. Don’t take that as the final word.
You have appeal rights. You can:
- File a Higher-Level Review if you believe the VA made a mistake based on the same evidence
- Submit a Supplemental Claim with new and relevant evidence
- Appeal to the Board of Veterans’ Appeals, especially if you want a hearing or need a more formal legal process
Plenty of veterans have had their claims denied or underrated at first, only to succeed later with persistence and better evidence. The system might be slow and flawed, but it’s not impossible.
Bonus Tip: Keep Your Symptoms Updated
Even after your initial claim, things can change. If your incontinence worsens, if you start using an appliance, or if other secondary conditions arise—you can file for an increased rating. The VA doesn’t automatically update ratings. It’s on you to request a reevaluation with supporting documentation.
And don’t wait years to do it. The sooner you file for an increase, the sooner your rating—and your benefits—can catch up with reality.
Bottom Line
Filing a VA claim for prostate cancer residuals is part paperwork, part medical advocacy, and part knowing the system. But once you know what the VA is looking for and how to speak their language, you gain control. You can cut through the fog and make your case with clarity and confidence.
In the next section, we’ll talk about how to go beyond the base rating and access Special Monthly Compensation (SMC)and other benefits that may not be on your radar—but absolutely should be.
Special Monthly Compensation (SMC) and Additional Benefits
Now that you’ve got a solid grasp of how the VA rates prostate cancer and how to navigate the claims process, it’s time to talk about something that often flies under the radar but can be a game-changer for many veterans: Special Monthly Compensation, or SMC.
You might be thinking, “I already get disability compensation—what’s this SMC, and why should I care?” That’s a fair question. And the answer is simple: SMC is extra compensation for veterans with particularly severe disabilities or specific losses of function—and for prostate cancer survivors, that can mean real additional income and support.
What Exactly Is Special Monthly Compensation?
SMC is an additional tax-free benefit on top of your regular disability compensation. It’s designed to recognize that some conditions cause more serious impairments than the standard rating schedule captures. This is especially true for loss of use of a creative organ, which is VA-speak for impotence caused by prostate cancer or its treatment.
Why Does Erectile Dysfunction (ED) Matter for SMC?
As we touched on earlier, ED alone usually earns a 0% rating in the VA system. That might feel unfair given how deeply it can affect quality of life, but the VA’s reasoning is that ED does not affect your ability to work.
However, the VA recognizes that loss of sexual function is a serious disability in a different way. If your prostate cancer or its treatment results in complete loss of use of a creative organ, you may qualify for SMC(k).
This benefit is often overlooked because it requires a separate claim and specific medical evidence. But once granted, it can add hundreds of dollars monthly to your compensation.
What Else Does SMC Cover?
SMC isn’t just about ED. It can also compensate for:
- The need for aid and attendance (help with daily living activities like bathing, dressing, or feeding)
- The loss or loss of use of limbs or organs
- Anatomical losses or disfigurements that interfere with function
- Certain combinations of disabilities that create an even greater level of impairment
For veterans with prostate cancer, the most common relevant SMC is the loss of use of a creative organ, but if your residuals have led to other severe impairments—like urinary retention requiring permanent catheter use—that can open the door to aid and attendance benefits, which can significantly increase your monthly payments.
How Do You Apply for SMC?
Unlike the standard disability rating, SMC requires a separate claim. You’ll want to:
- Submit specific medical evidence confirming the loss of use of the creative organ or other qualifying conditions.
- Provide physician statements documenting the nature and severity of your condition.
- Include personal statements describing how the disability impacts your daily life.
Again, working with a VSO or VA-accredited attorney can be invaluable here. They know how to frame the claim so it fits the VA’s legal criteria.
Are There Other Benefits Related to Prostate Cancer?
Yes. Here are a few worth knowing about:
- Total Disability Based on Individual Unemployability (TDIU):
If your prostate cancer or its residual effects (such as incontinence or fatigue) prevent you from maintaining substantially gainful employment—even if your rating is less than 100%—you may be eligible for TDIU. This benefit pays at the 100% rate and can be a lifeline if work is no longer an option. - Healthcare Benefits:
VA healthcare enrollment is usually automatic with a 60% or higher rating, giving you access to treatment and medications related to your cancer and other service-connected conditions. - Aid and Attendance (A&A):
If your residual symptoms mean you need help with activities of daily living, you could qualify for additional financial support through the A&A program.
One More Important Question: Can You Have Both a 60% Rating and SMC?
Absolutely—and this is where it gets good. Your 60% rating for prostate cancer residuals and an SMC benefit for loss of use of a creative organ are not mutually exclusive. They stack. This means you can receive a 60% rating plus extra SMC payments, significantly boosting your monthly compensation.
Why Don’t More Veterans Know About SMC?
Because it’s complicated. It requires understanding VA legal definitions and navigating a claims process that’s separate from standard disability claims. Many veterans miss out simply because nobody told them it existed—or how to apply.
That’s why this guide doesn’t just want you to understand ratings and claims but also the full spectrum of benefitsavailable—and how to claim every dollar and support you deserve.
Common Challenges and How to Overcome Them
By now, you’re probably getting a clear picture: securing a 60% VA rating for prostate cancer isn’t At this point in your journey, you’ve probably realized that securing a 60% VA rating for prostate cancer isn’t simply a matter of having the diagnosis. It’s not enough to say, “I had cancer. It affected my life.” The VA system—by design—is procedural, legalistic, and evidence-driven. And that means even well-qualified veterans often find themselves denied or underrated because the system didn’t fully see their reality.
So where do things go wrong? In truth, many of the roadblocks aren’t about the severity of your condition—they’re about how it’s presented, documented, and interpreted within the VA’s framework.
Let’s explore a few of the most common pitfalls that veterans encounter, and more importantly, how to move past them.
First, there’s the issue of underreporting symptoms.
This is more common than you’d think, and often rooted in military culture. Veterans are used to pushing through pain, not complaining, adapting, and staying quiet about discomfort. But when it comes to a VA claim, that instinct to “tough it out” can backfire.
If you tell the C&P examiner you “leak a little,” but you’re changing pads five or six times a day? You’ve just undersold your own rating. The VA won’t chase you for the truth. They will rate you based on what’s in front of them—what you say, and what the documentation supports.
So the real challenge here is letting yourself be honest. That means being specific about the number of pads you use per day. That means talking about the embarrassment, the logistics of going out in public, the sleep you lose because of nocturia, the intimacy lost from ED. Not because you want sympathy—but because that’s how the VA understands how your condition affects your life.
Then there’s the matter of medical records—and what’s not in them.
Veterans often assume that if something’s been said in conversation with a doctor, it’s “on the record.” But that’s not always the case. VA raters rely heavily on documentation. If your physician’s notes don’t say you’re using pads or catheters, or don’t quantify how many times a day you’re changing them, then as far as the VA is concerned, those symptoms don’t exist.
The problem is, not all doctors speak VA. Many will chart “urinary incontinence” without spelling out the frequency or severity. That’s where you come in. You have to advocate for clarity. Ask your provider to document the specifics: how often you need to change pads, whether you use an appliance, whether your condition affects your ability to work, travel, or maintain daily function.
You’re not asking for special treatment—you’re asking for precision.
Another common frustration comes from the C&P exam experience itself.
Let’s be honest: many veterans leave their exam feeling like they weren’t truly heard. Maybe the examiner rushed through. Maybe you felt too uncomfortable to explain everything in detail. Maybe you thought, “This will be in my file already—they must know.” But often, they don’t. And unless you explicitly tell them, the nuances of your condition can slip through the cracks.
If your exam doesn’t reflect what you’re actually going through, you can push back. You can request a new exam. You can submit additional evidence—a bladder diary, a statement from your spouse, a personal declaration clarifying what was missed. The C&P exam may shape the VA’s initial decision, but it’s not the final word unless you let it be.
Service connection is another tricky hurdle, especially for those without presumptive exposure.
If you served in Vietnam and were exposed to Agent Orange, the VA likely presumes a connection between your prostate cancer and your service. But if you served outside that window—or your exposure isn’t on the VA’s list—you may be asked to prove the link yourself.
This is where a strong medical nexus letter comes in. It’s not enough to submit a doctor’s note that says, “He has cancer.” You need a qualified medical opinion—ideally from a VA-savvy oncologist or urologist—explaining that your cancer is “at least as likely as not” connected to your service. That phrase isn’t optional; it’s the VA’s legal threshold for approval. Without it, your claim might stall no matter how compelling your case is.
And finally, some veterans simply don’t know how the VA breaks down the ratings.
You might be changing pads five times a day, but if you don’t know that “more than four changes daily” qualifies you for 60%, you might not mention it—or you might settle for a 20% rating without realizing there’s more available to you. The rating criteria can seem technical, but knowing the difference between 20%, 40%, and 60% could be the difference between barely getting by and receiving meaningful, life-changing compensation.
So yes, it matters. The details matter. The language matters. Knowing the thresholds and how to speak to them gives you leverage in a system that doesn’t always make things obvious.
So what’s the antidote to all these challenges?
Persistence, preparation, and support.
Track your symptoms daily. Be relentless about documentation. Speak up during exams, and don’t be afraid to correct the record. Work with people who know the system—VSOs, accredited reps, attorneys if necessary. And above all, be patient but firm. The VA isn’t fast, but it is navigable. And with the right knowledge and the right allies, you can get the benefits you’ve earned.
Every missed detail, every misunderstood symptom, every undersold claim is money—and dignity—left on the table. You deserve better. Now you know how to claim it.
And for a broader personal dimension, some may find strength in Celebrity Stories About Prostate Cancer, which blend science with lived experience.
Resources and Support for Veterans
At this point, you’ve done the heavy lifting. You understand what goes into securing a 60% VA rating for prostate cancer—the eligibility, the rating criteria, the service connection, the claim process, the fine print of SMC. But even with all that knowledge, the process can still feel overwhelming. There’s a reason so many veterans get stuck or give up partway through. It’s not because they lack the facts—it’s because they try to go it alone.
Here’s the good news: you don’t have to. There’s an entire ecosystem of support out there, designed specifically to help veterans navigate this system and win the benefits they’ve earned. The trick is knowing where to look—and how to use that help effectively.
Let’s start with the Veterans Service Organizations, or VSOs.
These are nonprofit groups that exist for one reason: to assist veterans. And when it comes to VA claims, they’re some of your strongest allies. Organizations like the Disabled American Veterans (DAV), Veterans of Foreign Wars (VFW), American Legion, and Paralyzed Veterans of America have trained, VA-accredited representatives who know the system inside and out. They’ll help you file your claim, gather evidence, track your progress, and advocate on your behalf—all at no cost to you.
Think of them as your field guides. They don’t just understand the process—they’ve walked hundreds of veterans through it. And they know how to catch the details that can make or break a claim: an incomplete C&P exam, a weak nexus letter, a missed opportunity for SMC.
If you’re not already working with a VSO, that’s your first stop.
For more complex or disputed cases, VA-accredited attorneys and claims agents offer another layer of expertise.
These professionals are especially helpful if your claim has been denied, underrated, or tangled up in appeals. They know how to build a legal argument, gather expert medical opinions, and represent you at hearings before the Board of Veterans’ Appeals or the Court of Appeals for Veterans Claims.
And while attorneys may charge fees—typically only if they win your case—many veterans find that representation is worth the investment, particularly when long-term compensation is on the line. The key is choosing someone experienced in VA law, not just general disability claims.
But it’s not all about legal strategy. Living with prostate cancer and its aftermath can take a toll on your mental and emotional health—and that’s where peer support and community come in.
Whether you’re coping with physical changes, dealing with feelings of isolation, or processing a sense of loss—support groups can help. Many VA hospitals offer cancer survivorship programs and group therapy sessions specifically for veterans. There are also national organizations like ZERO – The End of Prostate Cancer and the Prostate Cancer Foundation, which offer online forums and in-person events where you can connect with others who’ve been through the same thing.
Don’t underestimate the power of shared experience. Sometimes hearing “Me too” from another veteran is more helpful than anything a doctor or lawyer can say.
And then there’s technology—often overlooked, but incredibly useful.
Tools like VA.gov and My HealtheVet allow you to manage your claims, access your health records, message your care team, and monitor your compensation status in real time. These platforms can seem clunky at first, but once you get the hang of them, they give you direct access to your VA data—without the endless phone tag.
Set up alerts. Download your decision letters. Double-check that your appointments and exams are logged. It’s one more way to stay in control.
Finally, don’t forget the people closest to you.
Spouses, family members, caregivers—they’re often the ones helping you change pads, attending appointments, noticing when symptoms worsen. Their perspective matters, and their statements can carry weight in your claim. If your wife has been doing laundry three times a day because of leakage, that’s evidence. If your son sees how often you avoid social outings, that’s evidence. These observations help paint a fuller picture of how prostate cancer is affecting your life, even if it doesn’t show up on a lab test.
So no—you don’t have to navigate this alone. You shouldn’t. The system is dense and often impersonal. But support is out there—practical, emotional, legal, medical. Your job is to reach for it. Ask questions. Accept help. Let people stand beside you the way you once stood beside your unit.
Because when you bring that support into your fight, everything changes.
Frequently Asked Questions (FAQ)
By this point, you’ve absorbed a lot—how the VA rates prostate cancer, the path to a 60% rating, service connection, claims, SMC, and the challenges that come with it. But questions often linger, some subtle, some pressing. Let’s tackle the ones veterans most commonly ask, so you don’t have to wonder if your question is too small or too complicated to ask.
1. What exactly qualifies me for a 60% VA rating for prostate cancer?
To hit that 60% mark, you generally need either to use a urinary appliance (like a catheter) or need to change absorbent materials more than four times a day. It’s about the real-life impact of your symptoms, not just the diagnosis itself.
2. How long does the 100% rating for active prostate cancer last?
The VA assigns a 100% rating while you’re actively receiving treatment and for six months afterward. After that, your rating is reevaluated based on residual symptoms.
3. If I have erectile dysfunction due to prostate cancer treatment, does that increase my rating?
ED itself usually gets a 0% rating because it’s considered not to affect work ability. However, you may be eligible for Special Monthly Compensation (SMC) for loss of use of a creative organ, which adds additional monthly benefits.
4. How can I prove my prostate cancer is connected to my military service?
If you served in a location with recognized exposures—like Agent Orange in Vietnam—your cancer is presumptively connected. If not, you’ll need a medical nexus opinion linking your cancer to service-related factors.
5. What if my symptoms fluctuate? Do I get rated based on the worst days or average days?
The VA looks at your typical daily symptoms but also considers fluctuations. If you regularly have days where you exceed the rating criteria (like changing pads more than four times), make sure to document that.
6. What happens if the VA denies my claim or assigns a lower rating than I think I deserve?
You have the right to appeal. This can involve submitting new evidence, requesting a higher-level review, or appealing to the Board of Veterans’ Appeals. Persistence and good documentation are key.
Closing Thoughts
You’ve made it through a lot of complex information—everything from how the VA rates prostate cancer to the nuances of securing a 60% disability rating, establishing service connection, navigating claims, and even digging into the extra benefits like Special Monthly Compensation. That’s no small feat. It shows you care deeply about your well-being and your rights as a veteran.
Here’s the truth: the VA disability system isn’t perfect. It’s often slow, confusing, and frustrating. But it’s also the mechanism that can provide you with critical financial support and access to care you deserve after serving your country.
Remember, your prostate cancer residuals are real, and they matter. Whether it’s frequent incontinence, the need for medical appliances, or the emotional toll of loss of function, your symptoms have weight—and the VA rating process exists to recognize that weight. But it only works if you advocate for yourself with clear, detailed evidence and don’t shy away from asking for what you need.
If there’s one takeaway, it’s this: knowledge is power, but persistence is your ally. Keep detailed records, seek help from Veterans Service Organizations or qualified attorneys, prepare thoroughly for exams, and don’t hesitate to appeal decisions that don’t reflect your reality. You’re not just fighting for compensation—you’re fighting for dignity, quality of life, and recognition.
Finally, lean on the community—whether that’s other veterans, support groups, or professional advocates. You’re not alone on this journey.
Thank you for your service. And thank you for trusting this guide to help you navigate the path ahead.










